pain relievers, anti inflammatories, antivirals, and antihistamines all manage
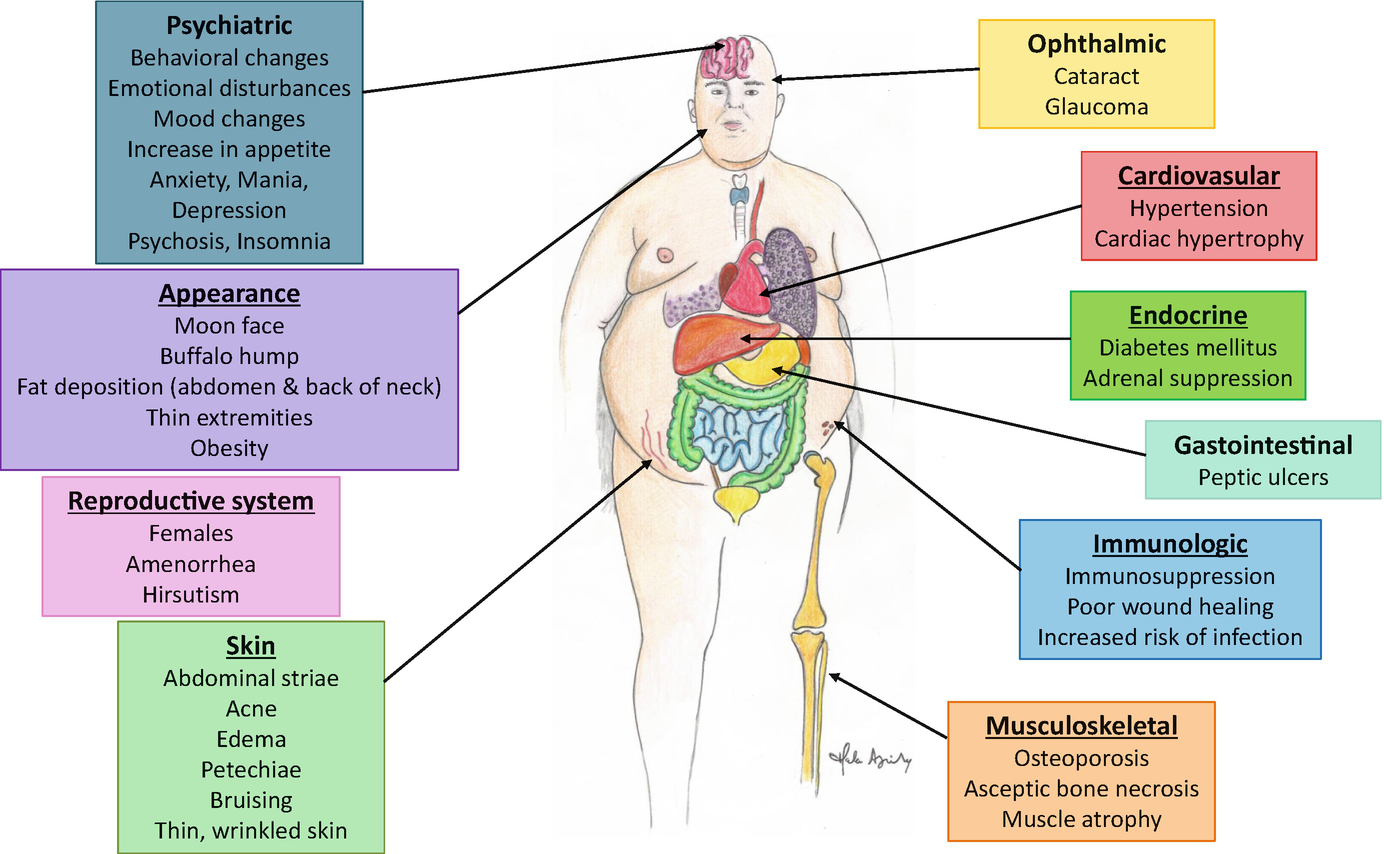
Warning: The NCBI website requires JavaScript to operate. Antihistaminic, Anti-inflammatory and Anti-allergic Properties of the Second Non-Protected Antihistamine Desloratadina: A Review of the EvidenceG. Walter Canonica1Allergy and Respiratory Diseases Clinic, DIMI, University of Genoa, Genoa, ItalyMichael Blaiss2Division of Clinical Immunology and Allergy Science Center, University of Resumen: The allergy cascade presents a widespread inflammatory and pro-inflammatory activation, robust cytokine and signaling of chemokines, and heterogeneous responses that lead to immune reactions. Histamine, a small peptide with inherent vasoactive properties, is released from granules contained in mast cells, basophils, lymphocytes and other reservoirs and interacts with histamine receptors to regulate numerous cell functions involved in allergic inflammation and immune modulation. Of known histamine receptors, the H1 receptor is very clearly associated with the enhancement of pro-inflammatory cellular activity and the enhanced effector function and is the main focus of suppressive therapy. Second-generation oral antihistamines, such as cetirizine, desloratadine, fexofenadine, levocetirizine and loratadine, are the pillars of allergy treatment, acting as highly specific and long-acting agonists in their unique receptor. Continuous identification of immune-impact cells and mediators involved in the allergic waterfall indicates that further research is needed to define the role of antihistamines as deloratadine in anti-inflammatory therapy. INTRODUCTIONHettamine, one of the most studied molecules in medicine, is a key mediator in allergic rhinitis (AR) and urticaria. Interacting with a single group of membrane receptors widely distributed in subtypes of immune cells, histamine participates in the intricate bidirectional messaging between cytokines and inflammatory cells or their precursors, facilitates the migration of cells to inflammatory sites, stimulates lymphocyte activity, modulates aspects of eosinophilic, neutrophilus behavior and smaller cells () and is directly involved in the disorder. Larger cell mediators, including cytokines, cause degranulation and contribute to bidirectional messaging with other inflammatory cells or their precursors, lymphocyte activity and immune cell migration to inflammatory sites. CNS, central nervous system; ECP, eosinophilic conical protein; ICAM, intracellular adhesion molecule; Ig, immunoglobulin, IL, interleukin; LT, leucotriene; MBP, bonding protein; MHC II, main histocompatibility complex; PGs, prostaglandins. Reprinted with permission of Baena-Cagnani et al. The H1-histamine receptor is very clearly associated with the modulation of the pro-inflammatory immune activity, and its interaction with histamine is the main focus of the suppressive therapy for AR and urticaria with the second generation H1-antihistamines such as cetirizin, desloratadine, ebastin, fexophenadine, levocetirizin, lotadina and ruratadine. As a class, these antihistamines are consistently effective for the relief of symptoms in histamine-mediated diseases. When used in recommended doses, second-generation antihistamines are essentially devoid of undesirable effects of the central nervous system (CNS) such as drowsiness, and are much less likely to cause other undesirable antihistamine side effects characteristic of first-generation antihistamines. Current management guidelines recommend second-generation antihistamines for front-line therapy for AR and hives. There are differences in pharmacology of second-generation individual antihistamines () and possibly in their individual capacity to suppress pro-inflammatory mediators associated with an allergic response. Some anti-inflammatory effects of antihistamines seem to require initial interaction with the histamine receptor while others are dependent on the receptor. It is necessary to study more thoroughly if these differences in anti-inflammatory pharmacology translate into clinically significant effects. TABLE 1Pharmacology of Select Second-Generation Antihistamines()Desloratadine, the active metabolite of loratadine, is a second-generation oral antihistamine with proven efficacy in randomized and controlled clinical trials, and a placebo-like safety and tolerance profile. In the European Union, desloratadine is indicated for the treatment of AR and urticaria intermittent and persistent in adults and children of ≥1 year. Desloratadine is approved in the United States for the treatment of seasonal AR in adults and children aged ≥2 and perennial AR and chronic idiopathic urticaria (CIU) in adults and children aged ≥6 months. In vitro studies, animal models studies and in vivo research show that desloratadine, similar to antihistamines such as levocetirizine (the active aantiomer of cetirizine) and others, inhibits a range of inflammatory mediators in addition to exercising a powerful H1 receptor antagonism. The present review will report recently on the available information that will expand the antihistaminic, anti-inflammatory and anti-allergic profile of desloratadine. H1-HISTAMINA RECEPTOR Four specialized and widely distributed receptors (H1, H2, H3, H4) mediate the effects of histamine. The local concentration of histamine and predominant type of histamine receptors that are being activated determines the type of response of the effectr that occurs. Most of the cells involved in inflammatory reactions express H1, H2, and H4, subtypes with the H1 receptor playing an important role in the enhancement of proinflammatory immune activity and fundamental effector responses for an allergic reaction; the H2 receptor, in contrast, appears to delete inflammatory and effector functions, while the data related to the H4 receptor's role in the immune response are limited. The H1 receptor is a transmembrane protein belonging to the G protein receptor family. Transduction of the signal from the extracellular environment to the intracellular occurs when the GCPR is activated after the union of a specific or agonist ligand. A subunit of G-protein later dissociates and affects intracellular messaging including the down signaling made through several intermediaries such as cyclic AMP, cyclic GMP, calcium and nuclear factor kappa B (NF-κB), a ubiquitous transcription factor designed to play an important role in immune cell quimotaxis, cell expression proinflation The classic activation model of the receptors requires binding by a specific ligand, or agonist. Progress in understanding the behavior of histamine receptors has established that histamine receptors can exhibit inherent and spontaneous activity ("constitutive activity") that is independent of the occupation of receptors by an agonist. A spontaneously activated histamine receptor interacts with your intracellular effector system through your typical intermediary, and causes a downstream event even in the absence of histamine binding. The concept of constitutive activity has led to a reclassification of drugs that operate in the H1 receptor. Antihistamines that combine with the inactive form of the receiver can be considered "inverse players", stabilizing the behavior of the receiver in the inactive state and reducing the population of receptors that exhibit constitutive activity. For example, the H1 receptor promotes NF-κB in a constitutive and agonist-dependent manner and all clinically available H1 anticists inhibit the H1-receptor-mediated constitutive production of NF-κB; an inverse H2-agonist or an H3 antagonist have no effect (). The ligadas that have no effect on the basal levels of constituent activity of the receptors, but which interfere with the union of agonists are considered "neutral antagonists" under this scheme. Importantly, because antihistamines may behave theoretically as reverse agonists or neutral antagonists, they are rather described as H1 antihistamines rather than H1 receptor antagonists. H1 receptors can be activated by an antagonist, such as histamine (A) or spontaneous or constitutive basal display, activity in the absence of ligand (B). Antihistamines repress both histamine-induced activity and constitutive activity, finally restoring the receiver to an inactive state (C). AH, antihistamine; H, histamine. Desloratadine: Antihistaminic, Anti-Inflammatory and Anti-allergic EffectsAffinity for the H1 Desloratadine receptor unites avid and not competitively to a recombinant human receiver H1, showing 52, 57, 194, and 153 times more potency for interaction than cetirizine, ebastine, fexofenadina Once deloratadine is tied, the dissociation of the receiver is slow; only 37% of desloratadine has no limits at 6 hours, suggesting pseudo-reversibility and supporting a prolonged duration of the action. As a second-generation antihistamine, desloratadine demonstrated reverse agonism, reducing downstream messaging by spontaneously active receptors. In a study, desloratadine effectively inhibited the signaling of a constitutively active H1 human receptor associated with NF-κB formation, reducing NF-κB basal activity to a greater extent than the equivalent concentrations of cetirizin, fexofenadine, loratadine or pirilamine. In addition, desloratadine was more powerful than comparers to block the increase of the NF-κ B after activation of the receiver by exposure to histamine. Effects on Immune Cells: Eosinophic Activation, Migration and SurvivalEosinophils, key-effect cells in the allergic response, are recruited from circulation to inflammatory activity sites where they participate in immune reactions and secrete a series of preformed cytoxic proteins (main basic protein, cationic protein, peroxidase, neurotoxin protein). Eosinophiles also produce cytokines, chemokines, leucotriene and neuromodulators. Dechloratadine may have effects on eosinophil chemicals, precursors, activation and survival. Desloratadine reduces the expression of NF-κB, a well-known RANTES inducer (regulated on activation, normal T cells expressed and secret), a major chemical for eosinophilics, monocytes and lynchites t. RANTES promotes eosinophilic activation and the release of histamine from basophiles. Desloratadine inhibited the release of RANTES by the epithelial lines of nasal polyps in response to the tumor necrosis factor (TNF), eosinophilic cationic protein and activated mast cells; this inhibition was also reflected in the production of triptase and leucotriene C4. In an investigation by enrolling atopic individuals with persistent asthma randomized to multisemane treatment with desloratadine or an oral steroid, both drugs significantly reduced the expression of mRNA specific to chemokines involved in T-cell signaling and activation of eosinophilic or lowfilo, including RANTES, inflammatory macrophagus protein (MIP)-1 β, and MIP α. The number of eosinophil/basophil progenitors (Eo/B) in peripheral circulation usually falls into atopic individuals, as these cells migrate to sites of inflammation through chemotraction, vascular adherence and extravasation. In a randomized placebo-controlled study of 45 subjects with symptomatic and seasonal AR treated with desloratadine (20 mg daily) or placebo, desloratadine receptors showed a significantly higher increase in peripheral Eo/B blood for the first 2 weeks of treatment compared to given placebo subjects. In addition, a statistically significant decrease in nasal lava eotaxine was found in the deloratadine group compared to placebo, which can support the concept that desloratadine blocks the migration of these cells from circulation to sites of inflammation within the nasal tissue. In a study that evaluates eosinophilic survival at the site of inflammation of the upper respiratory tract, the survival of peripheral blood eosinophils incubated with human epithelial cells conditioned media of nasal mucosa communication or nasal polyp tissue was reduced depending on the dose after pre-incubation with deloratadine. Effects on immune cells: mast cells and basophiles Antihistamines relieve the symptoms of AR and urticaria mainly by competing with histamine in the H1 receptor; emerging evidence indicates that antihistamines may also inhibit the degranation of smaller cells and subsequent release of histamine. The masculine and human basophil cells exposed to desloratadine show a reduction in the production of central cytokines to inflammatory responses. In a report, desloratadine reduced the phorbol 12-myristate 13-acetategogue-stimulated mast cell release of interleukin (IL)-3, IL-6, TNF-α, and granulocyte-macrophage colony-stimulation factor (GM-ClorSF) by 32.1, 32,6, 64.5, and 27.8% were easily tested In the highest desloratadine concentration (10−4 M), the inhibiting effect for anti-IgE, substance P and calcium ionophorus (50.7, 48.0 and 26.7% inhibition; P IL-4 is a growth factor of B lymphocytes and an important mediator of the allergic response, involved in the presentation of antigens and cytokine production. Human basophiles are an important source of IL-4 produced in experimental immune cell cultures. In an investigation, enriched derogations with lowfilo were incubated with several desloratadine concentrations for 15 minutes before stimulation with antibody anti-IgE, calcium ionofre, IL-3 or forbol ester. Notably, dechloratadine was almost 6 to 7 times more powerful in preventing secretion of IL-4 and IL-13 induced by anti-IgE than in inhibiting the release of histamine and leucotriene C4. After the pretreatment of desloratadine, IL-4 mRNA was inhibited by both 80%. These results are consistent with an earlier evaluation of the inhibiting effects of desloratadine and steroids (budesonide and dexamethasone) on the release of mast cells from IL-4, IL-6, IL-8, GM-CSF, and TNF-α after secret stimulation. Desloratadine showed less inhibition of cytokine compared to a glucocorticoid, but statistically significant (P Effects on Immune Cell AccessionDesloratadine has effects on the adherence of immune cells activated to endothelial and epithelial tissues. Desloratadine inhibits the in vitro expression induced by histamine of the P-selectine (implied on the adhesion and migration of neutrophils and eosinophils) and leads to a decrease in the production of IL-6, IL-8 and IL-8 mRNA. Incubated nasal epithelial cells with desloratadine for 24 hours show a significant decrease in the expression of the intercellular adhesion molecule (ICM)-1 (implied on the activation of the nasal epithelial cell) after exposure to histamine. Effects on inflammatory mediators In the first study to evaluate the possible anti-inflammatory activities of desloratadine in human epidermal cells, normal skin's keratinocytic cultures were activated by interferon (IFN)-γ in the absence or presence of desloratadine and evaluated for the release of RANTES, CXCL8, CCL17/TARC and CXCL10. The dose of desloratadine inhibited the constitutive and induced release of RANTES, CXCL8, and CXCL10. In addition, the keratinocyte supernatant was evaluated at 48 hours for its ability to attract types of immune cells. The dose of desloratadine reduced the migration of T-helper (TH)1 and TH2 cells to IFN-γ-stimulated keratinocytes and inhibited the release of chemicals induced by IFN-γ for human neutrophils and eosinophils. The eosinophilic trafficking associated with RANTES demonstrates the most significant reduction. In this study, the concentrations of desloratadine (1–100 μM) required for cytokine inhibition were higher than those considered to be achievable in plasma at a typical dose of 10 mg/d. In Vivo Investigation Cold Erticaria: Dose-dependence of anti-inflammatory and antihistaminic effects While in vitro findings strongly suggest that desloratadine has an anti-inflammatory capacity directed against important cytokines, the clinical relevance of these findings using standard doses remains unclear. Many of the reported anti-inflammatory effects of desloratadine are seen with higher doses than standard in the experimental configuration. On the other hand, an open and uncontrolled in vivo investigation of standard-dose desloratadine given to subjects with seasonal AR and concomitant asthma did not document a significant reduction in any mediator examined (IL-4, IL-8, IL-10, tumor growth factor-β) after 4 weeks of treatment. In a prospective, randomized, double-blind, crossover, 30 subjects with acquired cold urticaria (ACU), a disease in which clinical characteristics are due to the release of mast cell mediators in response to the cold, received placebo, desloratadine 5 mg, or desloratadine 20 mg each day, each for 7 days, separated by 14-day washing periods. After the cold provocation, the urtical reactions with three-dimensional digital images and thermogram were evaluated; the critical temperature and critical stimulation thresholds were measured. High-dose dechloratadine significantly improved the objective signs of the ACU and significantly reduced the severity of the ACU injury to desloratadine 5 mg without any concern of safety or adverse tolerance. These results strongly suggest that the antihistaminic and anti-inflammatory effects of desloratadine increase clinically relevant to the escalation of doses, and support the current guidelines that recommend the escalation of desloratadine doses for the treatment of ACU. DISCUSSIONH1 receptors are expressed in many types of cells, including smaller cells, basophiles, dendrite cells, endothelial cells and smooth muscle cells. Histamine stimulation causes the cardinal symptoms of an allergic response. The presence of histamine regulates the population of histamine receptors, and regulation is likely to be a continuous process while histamine is present. Receptor regulation is experimentally blocked by the presence of antihistamines. In addition, H1 receptors can demonstrate a spontaneous and constitutive signal even in the absence of histamine stimulation. H1 receptor antagonists effectively reduce allergy symptoms and reduce the signaling of constitutive and histamine-stimulated receptors. Desloratadine, a second-generation H1 receptor antagonist, has demonstrated clinical effectiveness in a range of conditions mediated by histamine and a placebo-like safety and tolerance profile. It has the longest half-life of any of the second-generation antihistamines and joins the H1 receptor with the highest affinity, dissociates slowly, shows non-competitive antagonism and reverse agonism, and effectively modulates allergic phenomena mid by histamine associated with AR and hives. Desloratadine does not feed on adults and without muscarinic side effects. It should be noted that other second-generation antihistamines have antiallergic, antihistamine and anti-inflammatory effects similar to those of desloratadine. In a series of pilot studies in subjects with persistent allergic rhinitis (PER), Ciprandi et al. investigated the effects of several of the most recent second-generation antihistamines on nasal congestion, nasal air flow and allergic inflammation. Rupatadine significantly improved nasal congestion (P = 0.0015) and increased nasal airflow (P = 0.0025) in 20 subjects with PER. Ebastine treatment in 20 patients with P also significantly improved nasal congestion (P = 0.0025) and nasal airflow (P = 0.0001). Desloratadine and levocetirizine improved nasal airflow in 30 patients with P = ns and P. Also mention should be made of some limitations of this review. The distribution volume (Vd) of √100 L/kg desloratadine is much higher than that of other second-generation antihistamines, which can counteract its affinity of higher receptors. You are the apparent volume in which a certain dose of the medication is distributed in the body at the equilbrium. However, the occupation of the receptors is due to several factors that are not the volume of distribution: total plasma concentration of the drug, which is related to the dose of the agent, its bioavailablity and its average plasma life. The level of occupancy of the receptors also depends on the degree of binding of plasma proteins, or the free concentration of plasma available for the receptor; percentage of proteins binding for deloratadine is comparable to other second generation agents (). Finally, our search did not reveal randomized controlled studies published with in vivo data showing the anti-inflammatory response in AR for desloratadine or other second-generation antihistamines. Rather designed studies are needed to determine the effects of these second-generation agents in the inflammatory response in AR patients. CONCLUSION The biochemical and effective pathways caused by the allergic response offer many potential goals and mechanisms by which desloratadine can modulate the activity of histamine receptors, inflammation cytokines and chemokines, or stimulate inflammatory cell migration and survival. In vitro data support anti-inflammatory effects of desloratadine in inflammatory cell function and mediator release. However, these studies often use desloratadine concentrations that are higher than what is clinically achieved in the recommended dosage. Inhibition dependent on the dose of inflammatory response in vitro suggests that the escalation of desloratadine doses can achieve a more potent anti-inflammatory response. The accumulation of information suggests that desloratadine can modulate aspects of inflammation through mechanisms other than the H1-histamine receptor blockage. Possible mechanisms hope that further research will be undertaken. ACKNOWLEDGMENTSFinancial support for this review was provided by Schering-Plough Corp., now Merck & Co., Inc., Whitehouse Station, NJ. Editorial assistance was provided by Patricia C. Abramo and Karl Torbey, MD, AdelphiEden Health Communications. This assistance was funded by Schering-Plough Corp. REFERENCESFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA

Focus On Pharmacology | Management of Chronic Pain in Cats

Pain medications and coronavirus (COVID-19): Do they work?
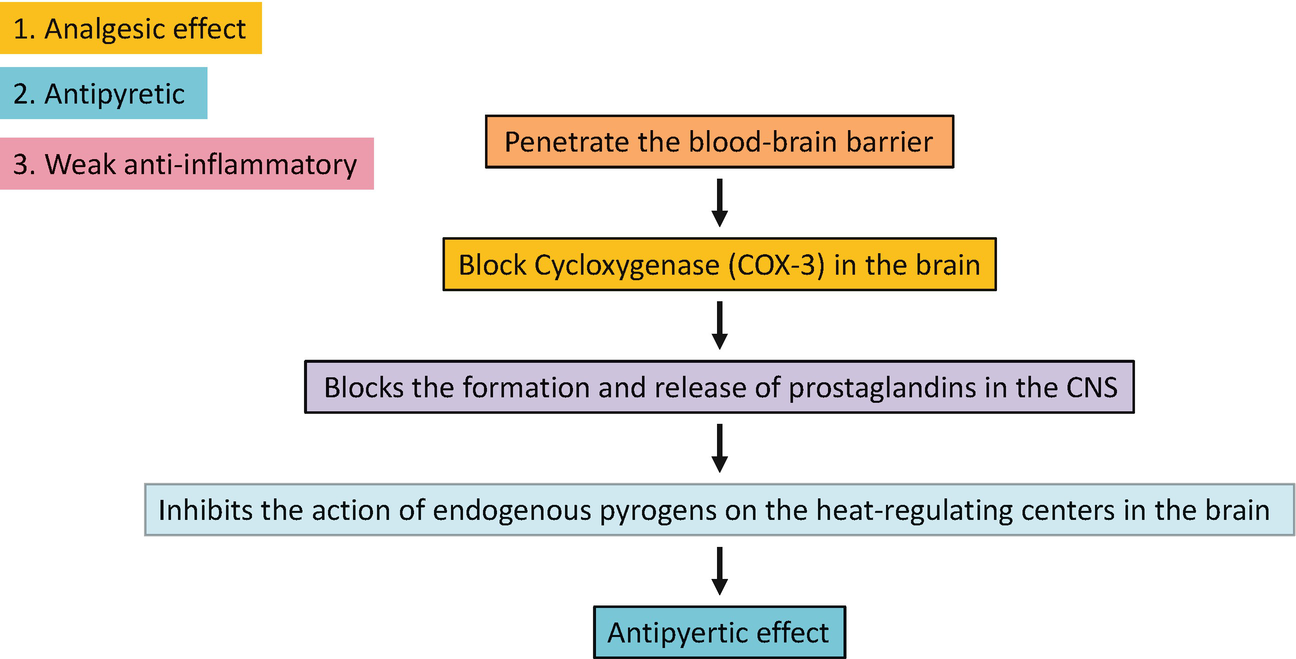
Pharmacotherapeutic Approaches in Oral Medicine | SpringerLink

Medicines that fight COVID-19: What to know

Pharmacotherapeutic Approaches in Oral Medicine | SpringerLink

Pain medications and coronavirus (COVID-19): Do they work?

Pain: Assessment and Treatment Using a Multimodal Approach | Springer Publishing
The Common Cold: A Review of OTC Options
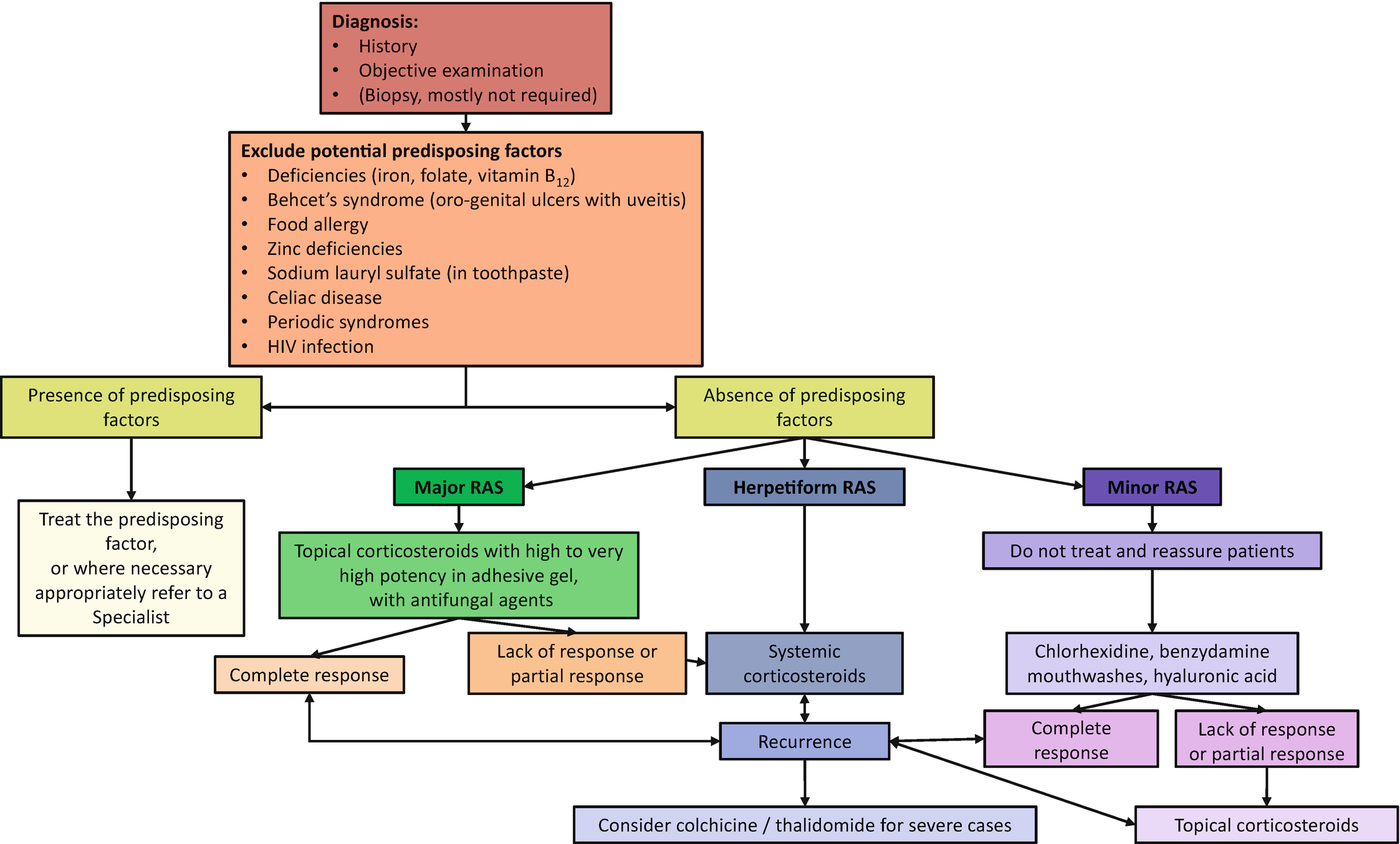
Pharmacotherapeutic Approaches in Oral Medicine | SpringerLink
/shingles_symptoms_IL-5aec997c8e1b6e0039a1df31-f560011d41fa4a20907723462634c617.png)
How Shingles Is Treated

Herpes Zoster and Postherpetic Neuralgia: Prevention and Management - American Family Physician
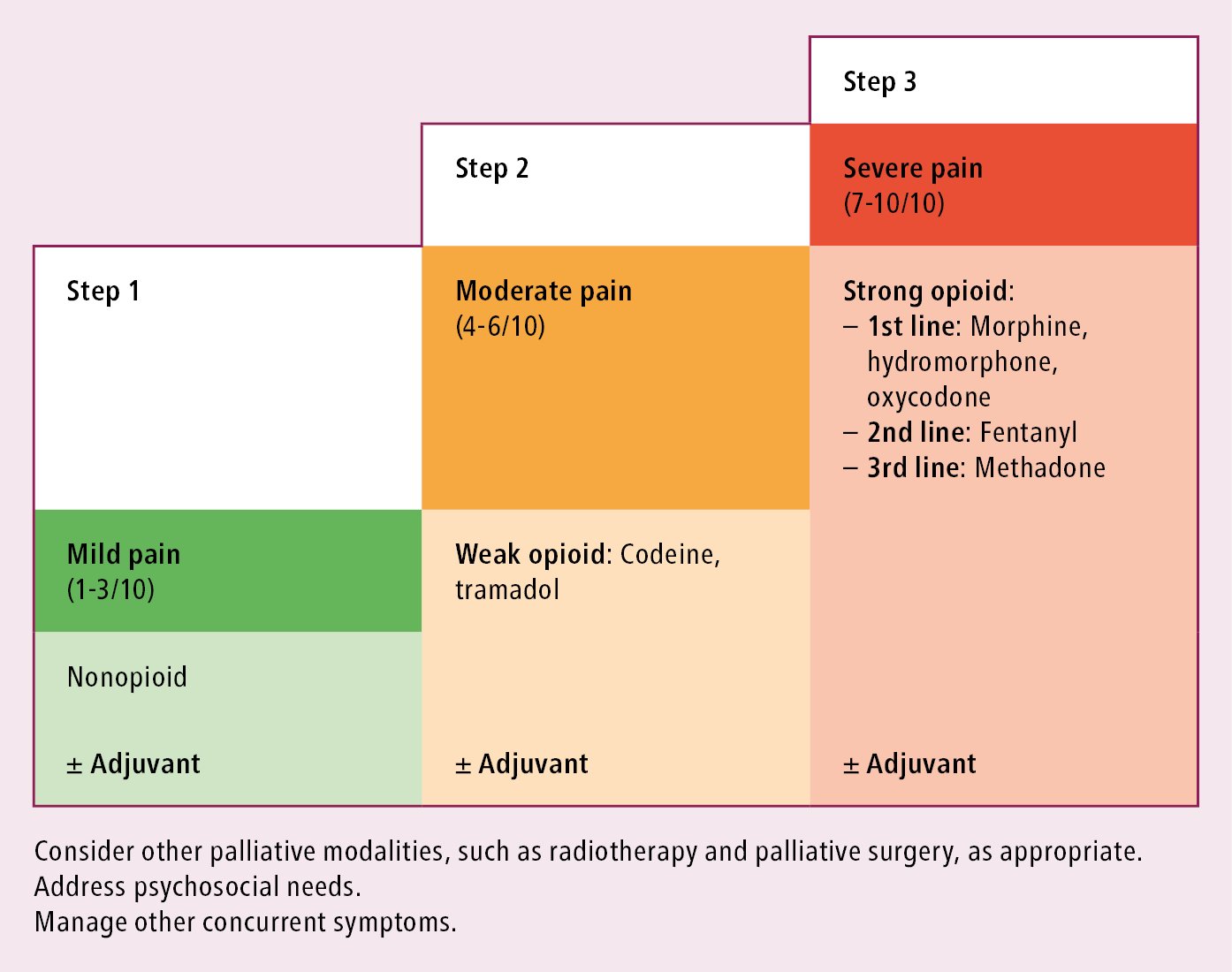
Pain Management: Basic Principles - Signs and Symptoms - McMaster Textbook of Internal Medicine

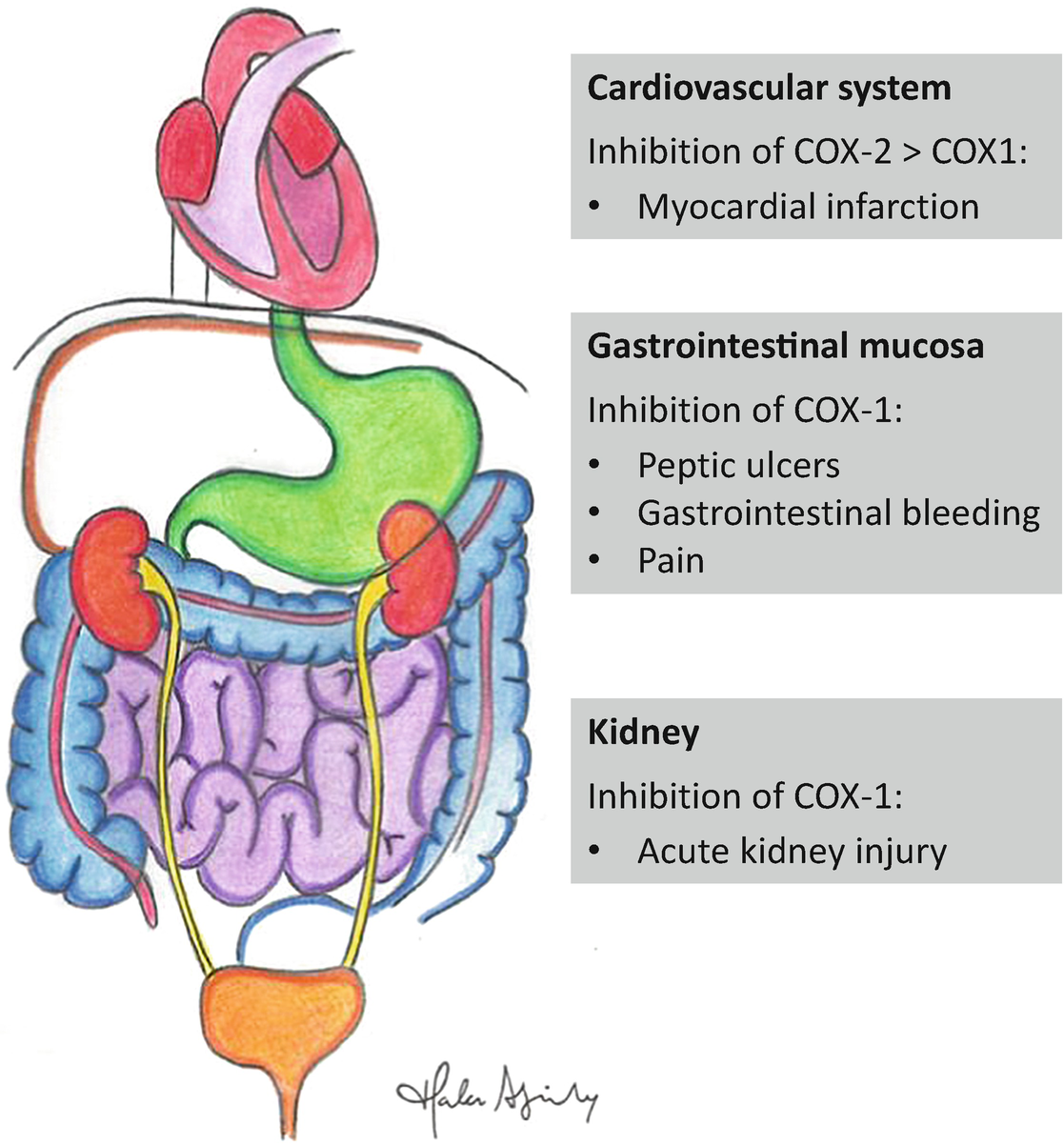
Over-the-Counter Anti-inflammatory Drugs: Types, Side Effects & More

Over-the-Counter Anti-inflammatory Drugs: Types, Side Effects & More

Management of Opioid Use Disorder in the Emergency Department: A White Paper Prepared for the American Academy of Emergency Medicine - Journal of Emergency Medicine
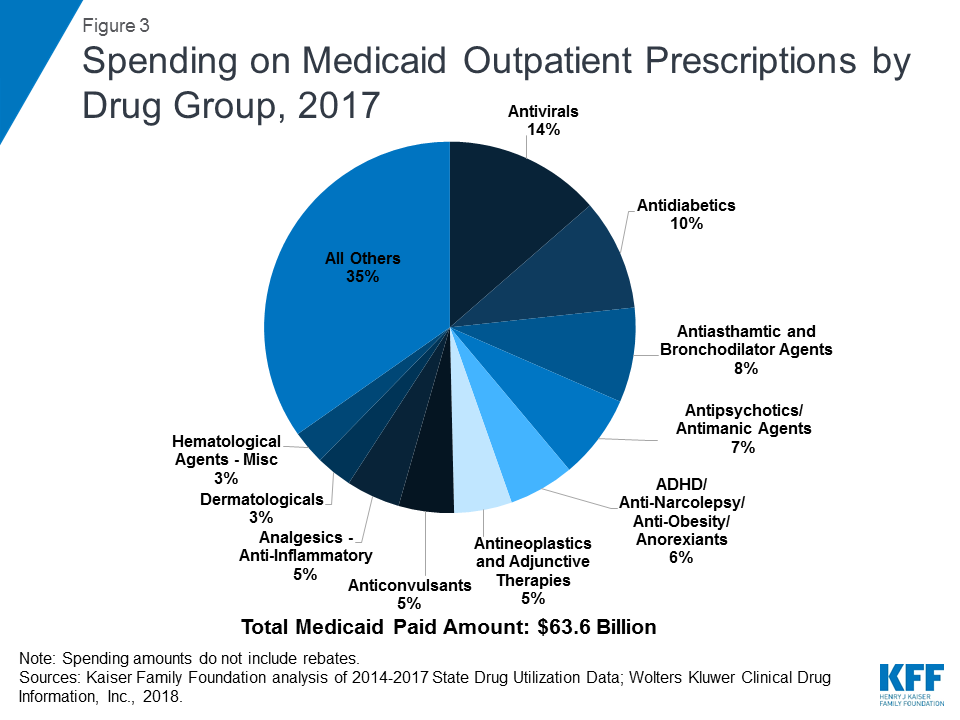
Utilization and Spending Trends in Medicaid Outpatient Prescription Drugs | KFF
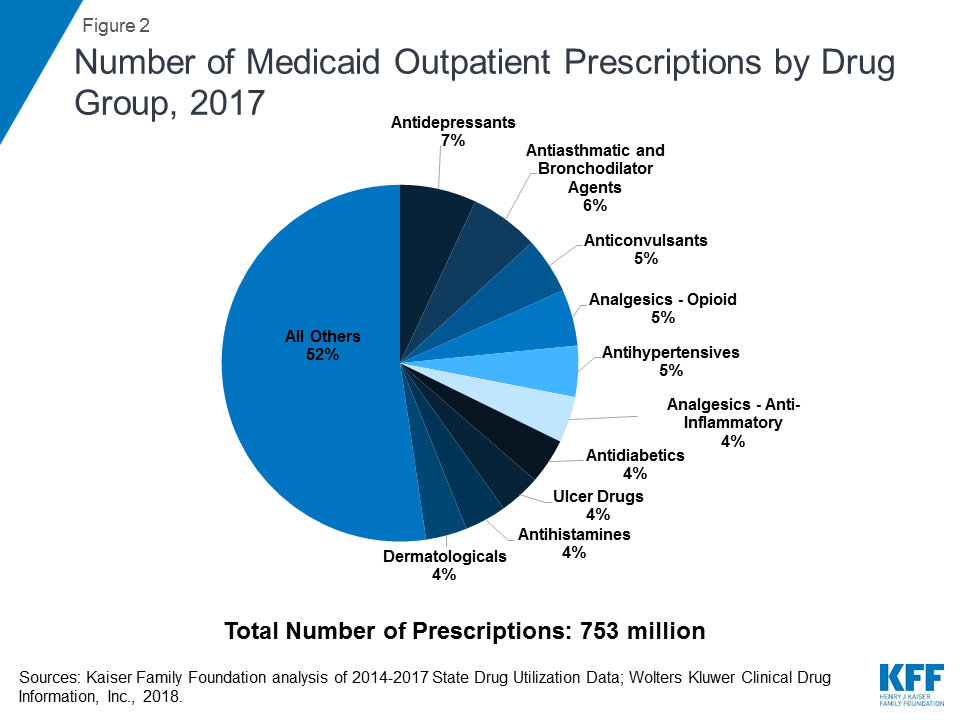
Utilization and Spending Trends in Medicaid Outpatient Prescription Drugs | KFF
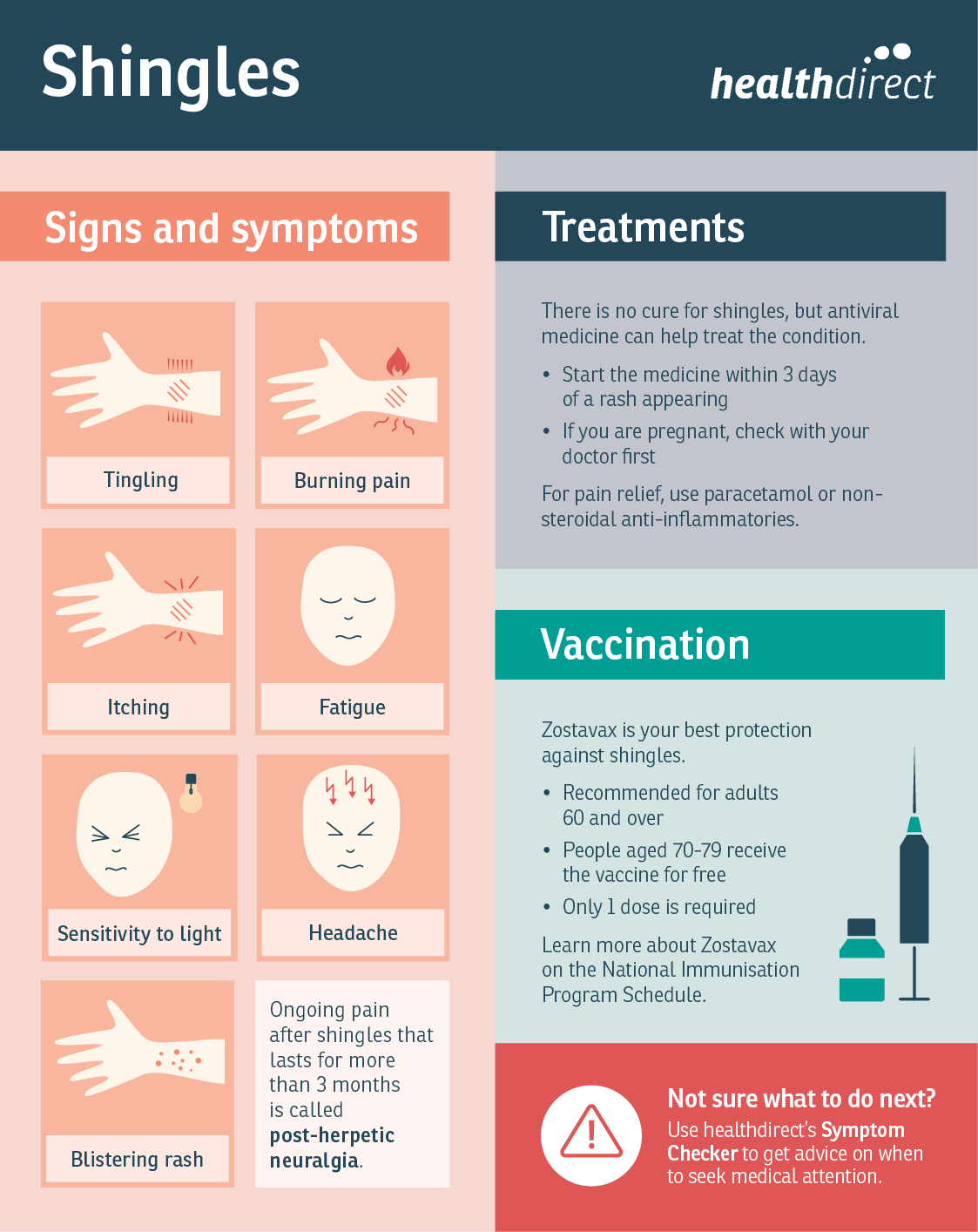
Shingles - treatments, symptoms and causes | healthdirect
.jpg)
What to do when medication makes you sleepy - Harvard Health
Pharmacotherapeutic Approaches in Oral Medicine | SpringerLink

NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) for Arthritis Pain
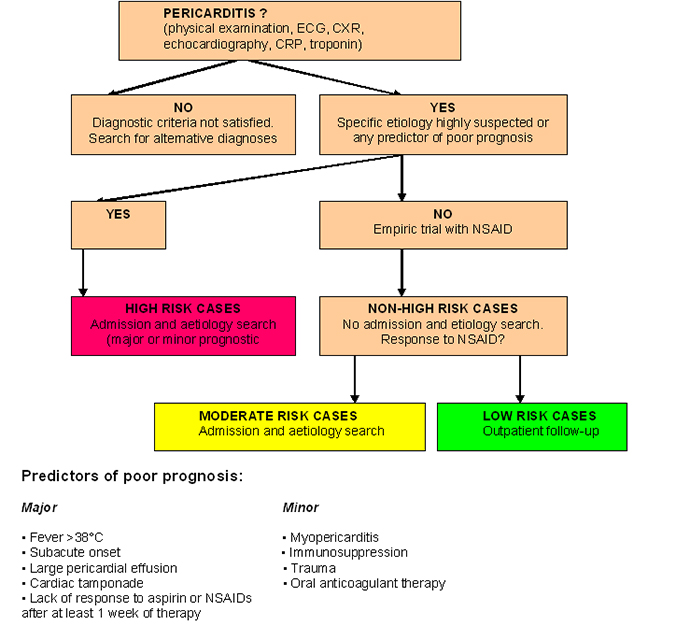
Management of acute pericarditis: treatment and follow-up
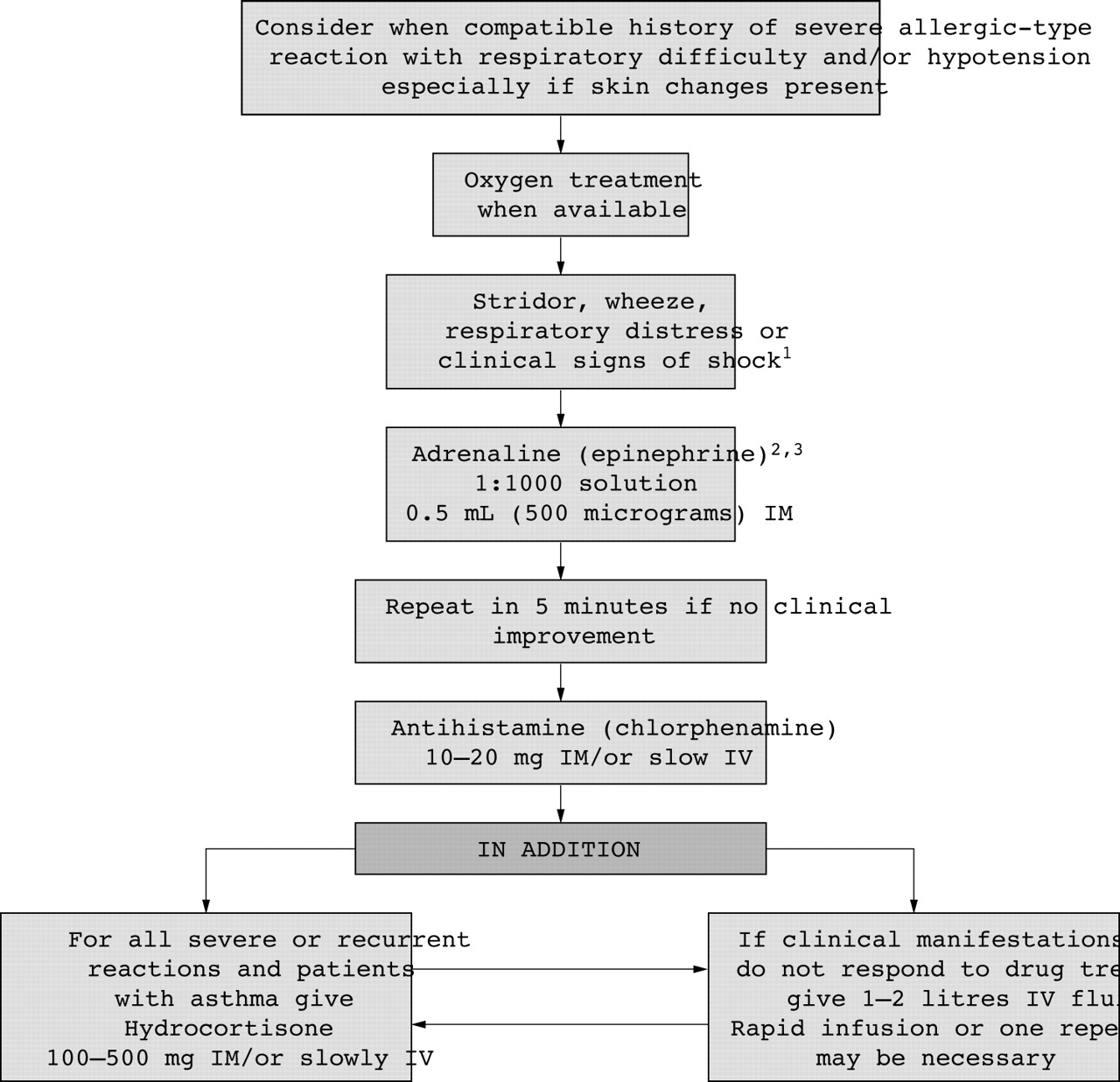
8 Management of allergy, rashes, and itching | Emergency Medicine Journal

Over-the-Counter Anti-inflammatory Drugs: Types, Side Effects & More
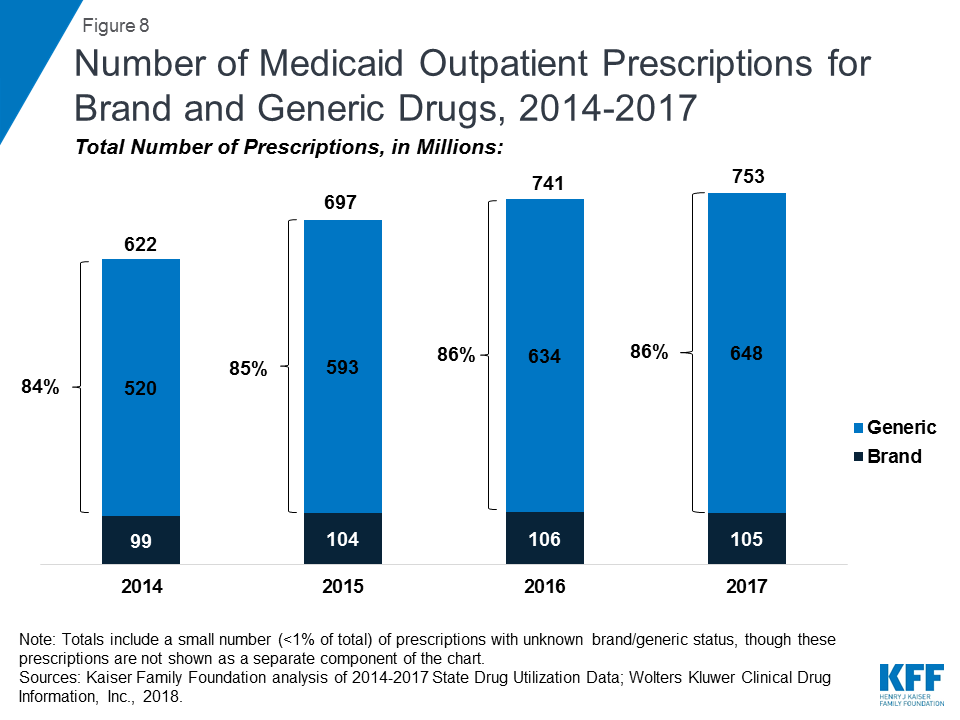
Utilization and Spending Trends in Medicaid Outpatient Prescription Drugs | KFF

Over-the-Counter Anti-inflammatory Drugs: Types, Side Effects & More
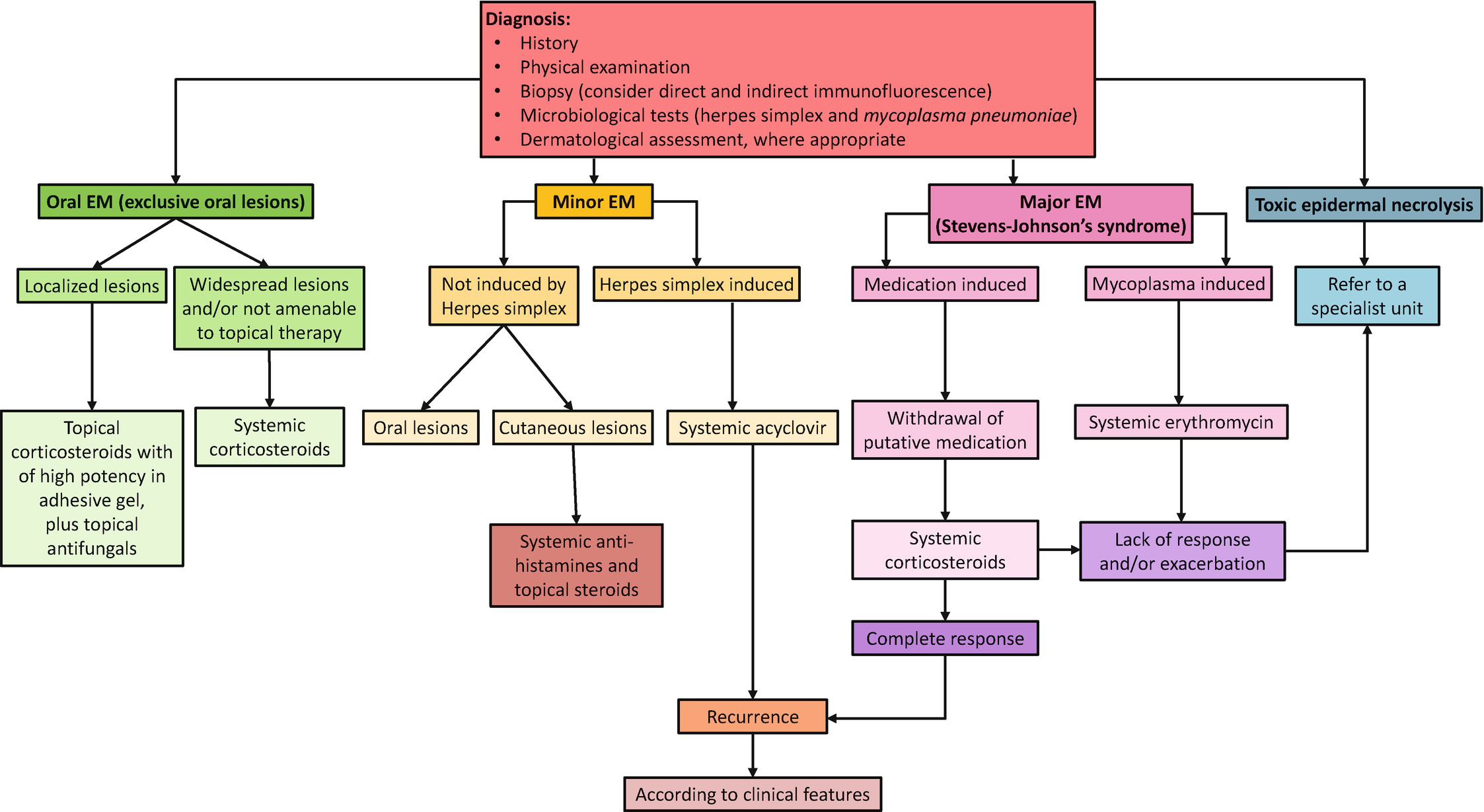
Pharmacotherapeutic Approaches in Oral Medicine | SpringerLink
The Common Cold: A Review of OTC Options

Herpes Zoster and Postherpetic Neuralgia: Prevention and Management - American Family Physician
Pharmacotherapeutic Approaches in Oral Medicine | SpringerLink

What scientists do and don't know about treating coronavirus

Delirium in Older Persons: Evaluation and Management - American Family Physician
![What's the Difference Between Cold and Flu? [Infographic] | Northwestern Medicine What's the Difference Between Cold and Flu? [Infographic] | Northwestern Medicine](https://www.nm.org/~/media/northwestern/healthbeat/images/healthy-tips/nm-cold-flu_preview.jpg)
What's the Difference Between Cold and Flu? [Infographic] | Northwestern Medicine

Arcoxia - NPS MedicineWise
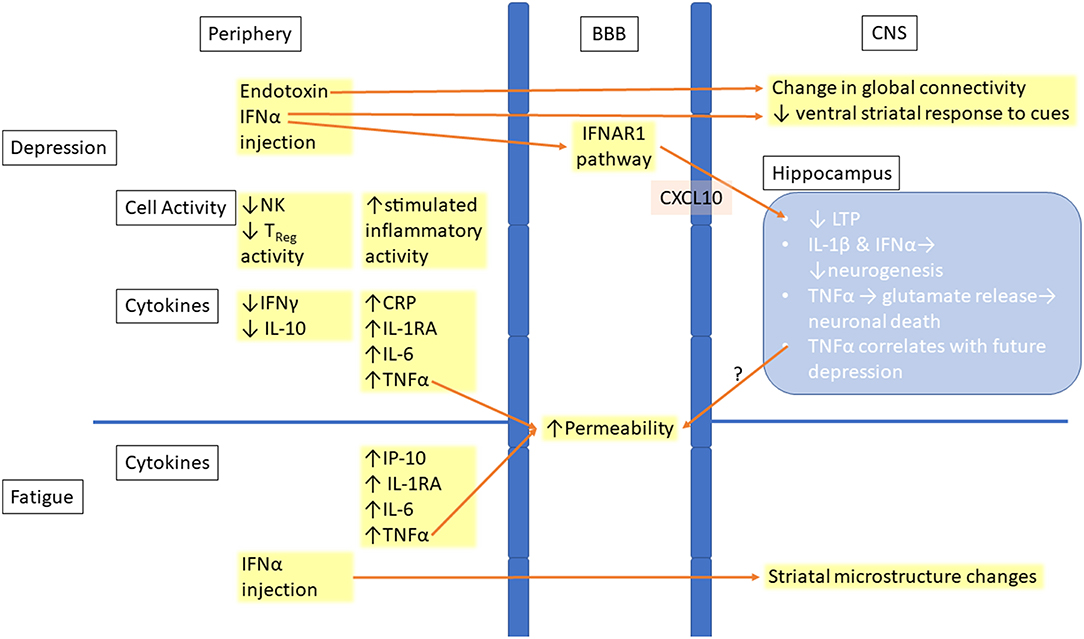
Frontiers | The Role of Inflammation in Depression and Fatigue | Immunology
Common hepatitis C symptoms and treatment side effects with tips for coping with them
Recommendations for the Management of Herpes Zoster
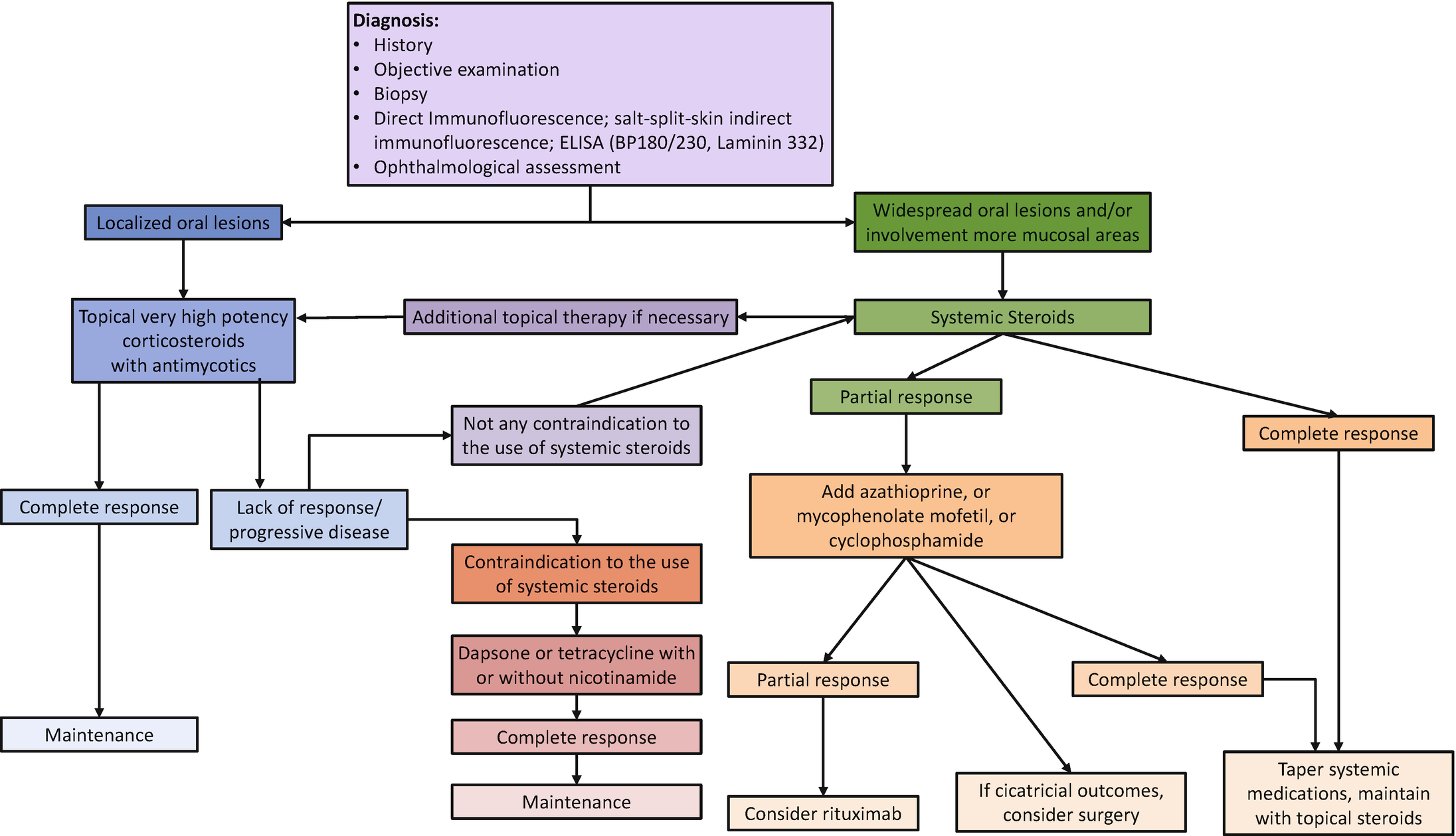
Pharmacotherapeutic Approaches in Oral Medicine | SpringerLink
Posting Komentar untuk "pain relievers, anti inflammatories, antivirals, and antihistamines all manage"