 Opioid-Induced Constipation: New and Emerging Therapies—Update 2016
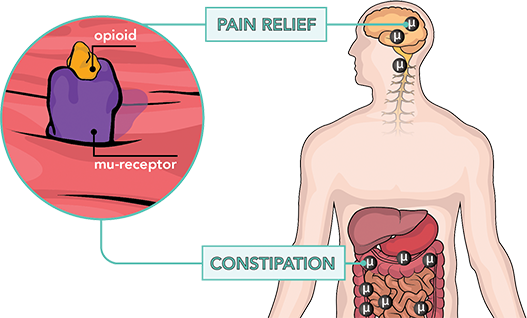
Opioid-Induced Constipation: New and Emerging Therapies—Update 2016Advert Comparison of the effectiveness of magnesium oxide and naldemedine in the prevention of opioid-induced constipation: a concept test, a single institutional, two arms, the open label, phase II, the randomized controlled trial: the MAGNET study Volume 21, Item number: 453 (2020) Volume 21901 Accesses1 Citations2 AltmetricAbstractBackground Patients taking opioids are known to develop opioid-induced constipation (OIC), which reduces their quality of life. The aim of this study is to compare magnesium oxide with naldemedine and to determine what is most effective in OIC prevention. MethodsThis randomized, prospective and randomized controlled trial began in Japan in March 2018. Initially, a questionnaire-based survey will be conducted for adult cancer patients who, concomitantly, initiated the treatment of opioids and the treatment of OIC prevention. Patients will be randomly assigned to a group of magnesium oxide (500 mg daily sleigh) or to a group of naldemedine (0.2 mg per day). Each medication will be given orally for 12 weeks. The primary endpoint is defined as any improvement of the scores in the Japanese version of the Patient Assessment of the Constipation Life Quality Questionnaire (JPAC-QOL) from the base to 2 weeks of treatment. Debate The primary end point is the change in the JPAC-QOL score from the baseline to 2 weeks of intervention. The key secondary end point will be the change in spontaneous bowel movements at 2 and 12 weeks of intervention. This study will determine whether magnesium oxide or naldemedine is more effective for OIC prevention. University Hospital Medical Information Network (UMIN) Clinical Trials Registry, . Registered March 25, 2018. BackgroundOpioids are used for the management of cancer pain [, ]; however, there are challenges associated with continuous opioid therapy, due to complications such as nausea, constipation, drowsiness and respiratory depression [,]. Constipation occurs in 15-64% of patients receiving strong opioid analgesics [,,,], and chronic constipation can occur more often in women (proportion between men and women, 1:2.2) and in older persons []. In patients with several cancers in Japan, the cumulative incidence of opioid-induced constipation (OIC) is lung, 48%; pancreas, 53%; colon, 60%; breast, 79%; stomach, 71%; esophageal, 60%, prostate, 50%; bladder, 50%; and others, 59% []. The long duration of opioid therapy is largely responsible for OIC [], and drug tolerance against OIC is seldom established, so the preventive administration of laxatives is important []. Symptoms of constipation (abdominal pain, fullness and loss of appetite) harm the quality of life of patients (QOL); therefore, OIC is a problem that is worth investigating. The traditional treatment of OCI consists of nondrug therapy that includes the consumption of high fiber diets or the administration of medicines such as laxatives. In Japan, clinical guidelines for gastrointestinal symptoms in cancer patients recommend osmotic laxatives []. A Japanese observational study reported that intake of preventive magnesium oxide attenuated OIC when patients started opioid therapy []. Therefore, osmotic laxatives, including magnesium oxide, are a conventional OIC treatment in Japan. OIC occurs when opioids act in μ-receptors in the intestinal nerves, reducing intestinal motility and fluid secretion [, ]. Both nondrug treatments and osmotic laxatives do not point to the underlying mechanism of the OCI [, ].During the years, little progress has been made in OCI treatment research []. Recently, μ-opioid receptor antagonists (PAMORAs) acted peripherally as effective in the treatment of OIC. Naldemedine is a PAMORA novel that develops for the treatment of OCI without affecting the central analgesy []. In addition, it has been reported that its safety and effectiveness are superior to placebo [, ]. Patients with OCI sometimes feel irritated, stressed and uncomfortable due to their restricted diet, or are ashamed of their frequent and long bath breaks, especially during social activities. Constipation harms the QOL of patients; therefore, preventive treatment is necessary. This study will compare magnesium oxide with naldemedine and determine which is most effective in OIC prevention. MethodsStudy Design This study is a concept test, a single institution, two arms, phase II, a randomized controlled trial that compares the effectiveness of magnesium oxide (500 mg a day) with that of naldemedine (0.2 mg a day) to prevent OIC for 12 weeks (the study of MAGNET). The primary end point will be the change in the Japanese version of the Life Quality Constipation Patient Assessment (JPAC-QOL) base score to 2 weeks of treatment. The study aims to recruit 120 adult patients with cohort cancer at Yokohama University Hospital. A flow chart of the study is shown in Fig. . The evaluations will take place at three points of time: on base and 2 and 12 weeks after the intervention, as shown in Fig. . Fig. 1Study flowchart Fig. 2Study schedule. All objectives will be compared between magnesium oxide and naldemedine. BSFS Bristol Stool Form Scale, CSS Constipation Scoring System, JPAC-QOL Japanese version of Patient Assessment of Life Quality Patients, PAC-SYM Evaluation of patients with symptoms of constipation, SBM Spontaneous bowel movements, SF-36 Short-form health survey The study will be conducted in accordance with the principles of the Japanese Declaration and Helsinki. The protocol was approved by the Ethics Committee of the Yokohama University Hospital on March 22, 2018. Standard protocol articles: Recommendations for the extension of the results notified by patients and their checklists were followed in the preparation of the protocol. This trial is registered with the Medical Information Network of the University Hospital (UMIN) Register of Clinical Trials under Identifier UMIN000031891. All participants should provide written informed consent. The protocol and all information provided to obtain informed consent were approved by the qualified Institutional Review Board/Independent Ethics Committee of the University of Yokohama prior to patient registration. The personal information of the participants will be kept in a closed cabinet and a password-protected hard drive at the University of Yokohama. The records will be kept for 5 years after the completion of the study and will then be destroyed by the data center. Endpoints of study The expected endpoints are listed in the table. The primary end point is the 2-week base JPAC-QOL change with magnesium oxide versus naldemedine intervention. JPAC-QOL consists of 28 evaluated questions using a score of 5 adjectival points from 1 to 5, with a lower score indicating a better result for QOL (table ) [,]. JPAC-QOL has proven to have acceptable reliability and validity to be used for psychometric evaluation in patients with functional constipation complaints []. Table 1 Table 2 Japanese version of Quality of Life Patient Assessment Side endpoints include the change of JPAC-QOL base scores to 12 weeks and the change in the evaluation of symptoms patients, constipation scotiade system, Rome IV criteria, Bristol hatch shape scale, spontaneous bowel movements (SBMs) and 36 stitches Short health survey at 2 and 12 weeks after the intervention began. Dosage Rationality A Japanese multi-institutional retrospective study reported that the prophylactic intake of 1000 to drug supply Both the doctor and the patient will be aware of the allocation of treatment. The doctor will prescribe magnesium oxide 1500 mg/day or naldemedine 0.2 mg/day according to the name of the medication provided by the patient's registration center. To improve adherence to interventional protocols, patients will be required to return unused tablets on the last visit, which will be recorded and recorded in medical records. Sample size estimate Our retrospective analysis of magnesium/naldemedina oxide in 10 patients with OCI at the Yokohama University Hospital showed JPAC-QOL changes of − 1.19 and − 0.76 in the naldemedine and magnesium oxide groups, respectively. We decide to calculate the size of the sample required to perform an appropriate analysis of the F variance test on the basis of this data. Assuming that this means changes in the JPAC-QOL score in the naldemedine and magnesium oxide groups would be − 1.19 and − 0.76, respectively, with a common standard deviation of 0.76, we determine that 51 patients would be required in each group to reach 90% of statistical power with a two-sided meaning level of 5%. To compensate for any abandonment, we propose an increase in sample size to 60 per group. To reach this sample size, a total of 120 patients will be required in the study. Eligibility Target study subjects are adult patients (20–85 years old) with cancer that will begin opioid therapy for cancer pain. There is no distinction in the type and location of cancer. The type, dose or frequency of opioid medication will not be limited in this study. The eligible subjects will be required not to use laxatives prior to the study's intervention. If severe OIC that cannot be controlled by magnesium oxide or naldemedina occurs during the intervention, senna use will be allowed. The inclusion and exclusion criteria are presented in the table. Table 3 Criteria for Inclusion and ExclusionRandomization and Masking Patients susceptible to meeting the criteria for inclusion and exclusion of detection will be invited to participate in the study of researchers. Patients will be randomly assigned in a 1:1 ratio to receive 500 mg of daily sleigh magnesium oxide or 0.2 mg of naldemedine once a day in the central registry center. Randomization will take place after the patient has signed the informed consent form. The principal investigator or researcher will be notified of the patient's identification number and the name of the drug by fax from the patient's registration center. To avoid a great bias, we will stratify patients by age (Control of adverse eventsThe researchers will be required to record all the adverse events (AEs) that occur during the study in the medical records, including information on the beginning and final date (if applicable), severity and severity of AE, the opinion of the researcher on the association with magnesium oxide or treatment of naldemedine, the measures adopted in relation to the known magnesium oxide The intensity of an AE will be classified according to version 4.0 of the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE), which includes the AE intensity classifications shown in the Table. Any abnormal results related to the treatment of study drugs will be reported weekly until the abnormality is resolved or otherwise explained. Table 4 Discontinued CriteriaThe treatment of study will be suspended when a 3rd or higher grade of severe E occurs according to version 4.0 of NCI-CTCAE, when oral compliance is Definition of the deviations of the protocol The deviations of the Protocol are defined as: Diagnosis of patients who were not randomized after the informed consent Risk: patients who do not meet the inclusion criteria or who meet the exclusion criteriaPatients who were not treated: patients who did not receive the study medicationFulfiment of criteria for disintegration: patients who met the criteria described in the decomposition protocol of studies The endpoints of secondary efficiency will be calculated as the mean difference from the baseline to 2 or 12 weeks. Security Assessment The AAs, dropout ratios and physical exams are the chosen safety evaluations of this test. Physical evaluations will be conducted and analysed through standard procedures at the University of Yokohama. Abandonment will be defined as oral compliance Statistical hypothesis The complete analysis set is defined as all patients who receive any amount of the study medication with initial information on the primary end point. The complete analysis set will be the primary analysis established for the effectiveness to be used as a patient population with intent to treat. For the primary end point, a variance analysis will be performed between the two groups to calculate the p value using Student t test. The p value will be significant in a two-sided significance level of 5%, and both the p value and the confidence intervals will be used to determine the statistical significance of our results. The t matched test or Wilcoxon signed-rank test will be performed for comparisons within the group before and after the intervention. The chi-quarela test will be used to evaluate the frequency of ATS, and the rate of compliance with the treatment will be calculated and compared to Fisher's exact test. The JMP software version 11.2.0 (SAS Institute, Cary, NC, USA) will be used for all statistical analysis. Full case analysis based on probability will be used for primary analysis, or a multiple imputation method will also be used to handle lost data as a sensitivity analysis. Management and data monitoring committees in processes The independent trial management and data monitoring committees will be located in the Department of Biostatistics, the School of Medicine of the University of Yokohama and the University Center of the City of Yokohama for clinical trials of novel and exploration. The management team will follow up on-site and meet with the person in charge of the facilities when necessary. The monitoring report will report any visit to the centre. In principle, the first patient will be monitored continuously throughout the trial, and, if no problem, every 10th patient will be monitored. To confirm that the necessary documents are stored properly, appropriate on-site monitoring will be carried out and, if any, corrective action will be taken. The result will be recorded in the monitoring report. The data monitoring committee will have access to the end-of-trial dataset, and there is no contractual agreement on the access restrictions of researchers to the dataset. DiscussionPatients with OCI report a QOL significantly worse than those who are not affected by OIC [, ], due to symptoms associated with abdominal pain, feeling fullness and loss of appetite, but their QOL improves after the resolution of symptoms []. JPAC-QOL is a reliable method to measure QOL for patients with constipation. A decrease in constipation can also be determined by the number of times a patient defecates using the SBM score, but evaluating patient comfort only by using this target index is difficult due to high inter-individual differences in defecation times. QOL improvement is particularly important in cancer patients, and therefore we choose the change in the JPAC-QOL score as the primary end point of this study. In this study, we chose magnesium oxide as a control because in Japan, its preventive intake is reported to dampen OIC when patients eventually begin opioid therapy [], and osmotic laxatives, including magnesium oxide, are used conventionally to treat OIC. Other laxatives, such as senna, lactulosa and sodium picosulphate hydrate, are also used, and all are effective. However, a systematic review of Miles et al. [] did not indicate evidence of superiority of a laxative or specific combination of laxatives for the management of constipation in palliative care patients. Similarly, Agra et al. [] reported no difference in the effects of senna and lactulose after observing the subjective index for more than 72 h and the number of days with defecation throughout the study. Magnesium oxide is used conventionally for the prevention of OIC in Japan; therefore, its long-term security is empirically established. In addition, magnesium oxide has advantages in terms of medical cost to 33.6 yen/day (1500 mg/day) over naldemedine, which costs 272,1 yen/day. Naldemedine may have the advantage of adherence with a required intake of once a day. There is a good number of OIC treatment studies, with only a few on the use of preventive laxatives against OIC. In addition, some limitations of our study are that it is done in a single center, its open label design and a potentially short treatment period (12 weeks). The justification for conducting this trial as an open label study is as follows: This test compares two drugs, which are already on the market and are used in clinical practice. Both agents compared in this trial are active drugs. The dual-management method is necessary to blind, and the logistics of using that method in a study, such as placebo manufacturing costs, drug management and drug dispensation, are difficult. This is an exploratory study. We have considered the need to stop the next phase using the dual administration method. Further research is encouraged. Dissemination The results of this study will be presented for publication in peer-reviewed international journals, and the key conclusions will be presented at conferences. The authorization shall be in accordance with the guidelines of the International Committee of Medical Journal Editors. Judgment Situation Protocol version: 1.0, 26 November 2017. Recruitment began on 22 March 2018, and was ongoing on 26 May 2020. Availability of data and materials Not applicable. Daily life activities Adverse events Bristol Stool Form ScaleConstipation Scoring System Japanese patient assessment of the quality of life questionnaire National Cancer Institute Common Terminology criteria for adverse eventsOpioid-induced constipation Evaluation of patients with symptoms of constipation Antagonistic receptor μ-opioids of peripheral actionCality of lifeSpontaneous bowel disease Ustekinumab does not increase the body mass index in patients with chronic plaque psoriasis: a prospective cohort study. Br J Dermatol. 2013;168:1124-7. . Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, Cherny N, et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations of AAC. Lancet Oncol. 2012;13:e58–68. . Poulsen JL, Brock C, Olesen AE, Nilsson M, Drewes AM. Evolution of paradigms in the treatment of opioid-induced intestinal dysfunction. Ther Adv Gastroenterol. 2015;8:360–72. . Morlion B, Clemens KE, Dunlop W. Quality of life and health resources in patients receiving opioids for chronic pain: a review of the place of oxycodone/naloxone. Clin Drug Investig. 2015;35:1–11. . Lazzari M, Greco MT, Marcassa C, Finocchi S, Caldarulo C, Corli O. Effectiveness and tolerability of oral oxycodone and the combination of oxycodone/naloxone in patients with opioid-naive cancer: a propensity analysis. Drug Des Devel Ther. 2015;9:5863–72. . Camilleri M. Opioid-induced constipation: challenges and therapeutic opportunities. Am J Gastroenterol. 2011;106:835–42. . Wirz S, Wittmann M, Schenk M, Schroeck A, Schaefer N, Mueller M, et al. Gastrointestinal symptoms under opioid therapy: a prospective comparison of oral release hydromorphone, transdermal fentanyl and transdermal buprenorphine. Eur J Pain. 2009;13:737-43. . Cook SF, Lanza L, Zhou X, Sweeney CT, Goss D, Hollis K, et al. Gastrointestinal side effects on chronic opioid users: results of a population-based survey. Aliment Pharmacol Ther. 2008;27:1224–32. . Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity and impact of opioid-induced intestinal dysfunction: results of a survey of American and European patients (PROBE 1). Med. 2009;10:35–42. . Yotoku M, Nakanishi A, Kanematsu M, Sakaguchi N, Hashimoto N, Koyama F, et al. The reduction of opioid side effects by prophylactic measures of palliative care equipment can result in better quality of life. J Palliat Med. 2010;13:401-6. Rosti G, Gatti A, Costantini A, Sabato AF, Zucco F. Opioid-related intestinal dysfunction: prevalence and identification of predictive factors in a large sample of Italian patients in chronic treatment. Eur Rev Med Pharmacol Sci. 2010;14:1045–50. Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004;99:750-9. Tokoro A, Imai H, Fumita S, Harada T, Noriyuki T, Gamoh M, et al. Incidence of opioid-induced constipation in Japanese patients with cancer pain: a prospective study of observational cohorts. Cancer Med. 2019;8:4883–91. Tuteja AK, Biskupiak J, Stoddard GJ, Lipman AG. Intestinal disorders induced by opioids and small intestine syndrome in patients with noncancer chronic pain. Neurogastroenterol Motil. 2010;22:424–30.e96. . Clinical guidelines for cancer pain management. 2nd edition 2014. Clinical Guidelines for Gastrointestinal Symptoms in Cancer Version 2017. Ishihara M, Ikesue H, Matsunaga H, Suemaru K, Kitaichi K, Suetsugu K, et al. Japanese study group for the relief of opioid-induced gastrointestinal dysfunction: a multi-institutional analysis effect of prophylactic medication for the prevention of opioid-induced gastrointestinal dysfunction. Clin J Pain. 2012;28:373–81. . Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary consensus statement by the working group on opioid-induced constipation. Neurogastroenterol Motil. 2014;26:1386–95. . Song X, Wang D, Qu X, Dong N, Teng S. A metaanalysis of naldemedine for the treatment of opioid-induced constipation. Expert Rev Clin Pharmacol. 2019;12:121-8. . Fukumura K, Yokota T, Baba Y, Arjona Ferreira JC. Phase 1, randomized, double-blind, placebo-controlled studies on the safety, tolerance and pharmacokinetics of naldemedine in healthy volunteers. Clin Pharmacol Drug Dev. 2017;7:474–83. . Webster LR, Yamada T, Arjona Ferreira JC. A randomized, double-blind placebo-controlled study to assess the efficacy and safety of naldemedine for the treatment of opioid-induced constipation in patients with non-cancer chronic pain. Dolor Med. 2017;18:2350–60. . Katakami N, Harada T, Murata T, Shinozaki K, Tsutsumi M, Yokota T, et al. Random studies of phase III and extension: efficacy and impacts on the quality of life of naldemedina in subjects with opioid constipation and cancer. Ann Oncol. 2018;29:1461-7. . Nakajima A, Seki M, Taniguchi S, Ohta A, Gillberg PG, Mattsson JP, et al. Safety and effectiveness of elobixibat for chronic constipation: results of a randomized, double-blind, placebo-controlled trial, phase 3 and an open phase 3 test, of a single arm, phase 3. Lancet Gastroenterol Hepatol. 2018;3:537–47. . Marquis P, De La Loge C, Dubois D, McDermott A, Chassany O. Development and validation of the assessment questionnaire for patients with constipation Quality of life. Scand J Gastroenterol. 2005;40:540–51. Mokhtare M, Ghafoori SM, Soltani-Kermanshahi M, Boghratian AH, Agah S, Sheikhvatan M. Reliability and validity of the Persian version of patient constipation- quality of life (JPAC-QOL) questionnaire. Gastroenterol Hepatol Bed Bench. 2017;10:289-94. Ishihara M, Ikesue H, Matsunaga H, Suemaru K, Kitaichi K, Suetsugu K, et al. A multi-institutional study that analyzes the effect of prophylactic medication on the prevention of opioid-induced gastrointestinal dysfunction. Clin J Pain. 2012;28:373–81. . Miles CL, Fellowes D, Goodman ML, Wilkinson S. Laxatives for the management of constipation in palliative patients. Cochrane Database Syst Rev. 2006;4:CD003448. . Agra Y, Sacristá A, González FM, Portuguese A, Calvo MJ. Senna effectiveness versus lactulose in terminal cancer patients treated with opioids. J Doin Symptom Manage. 1998;15:1-7. Recognition This work was partly supported by the palliative care team at the University of Yokohama. Financing This trial was conducted with funding granted by the Yokohama University Hospital, and no external funding was used. Author's information Anna Ozaki and Takaomi Kessoku also contributed to this work. Affiliates University of Japan and Japan You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in ContributionsAO, T. Kessoku, and AN conceived the study. T. Yamanaka, HI, and YI conducted the feasibility phase work. MI, T. Kobayashi, T. Yoshihara, YH, YO, KI, TH, MY, NK and SS will recruit patients and follow up. T. Kato will assign patients. MT will analyze data. All authors contributed to the writing of the manuscript, and all authors read and approved the final version. Correspondence to the correspondent .Ethic declarations Ethics and consent to participate The protocol was approved by the Ethics Committee of the Yokohama University Hospital (Approval Reference Number B180301006). The informed consent was obtained to participate in the trial of all patients, who will be informed of the results of the trial by the researchers. Consent for publication Not applicable. Competing interests The authors declare that they have no competing interests. Additional Information Editor's Note Nature remains neutral with respect to jurisdictional claims on published maps and institutional affiliations. Rights and permits Open access This article is licensed by Creative Commons Attribution 4.0 International License, which allows use, sharing, adaptation, distribution and reproduction in any medium or format, provided that you give appropriate credit to the original author(s) and source, provide a link to the Creative Commons license, and indicate if changes were made. Third-party images or other material in this article are included in the Creative Commons license of the article, unless otherwise indicated in a credit line to the material. If the material is not included in the Creative Commons license of the article and its intended use is not permitted by legal regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit . Renunciation of the public domain of Creative Commons () applies to the data available in this article, unless otherwise indicated in a credit line to the data. Open accessOn this article Cite this article Ozaki, A., Kessoku, T., Iwaki, M. et al. Comparing the effectiveness of magnesium oxide and naldemedine in the prevention of opioid-induced constipation: a concept test, a single institutional, two arms, the open label, phase II, the randomized controlled trial: the MAGNET study. Tests 21, 453 (2020). https://doi.org/10.1186/s13063-020-04385-021, Received: 05 August 2019 Accepted: 06 May 2020Published: 01 June 2020DOI: KeywordsPublication Trials ISSN: 1145-6215 Contact us BMC By using this website, you agree to our , , and politics. We use at the center of preferences. © 2021 BioMed Central Ltd unless otherwise indicated. Part of .
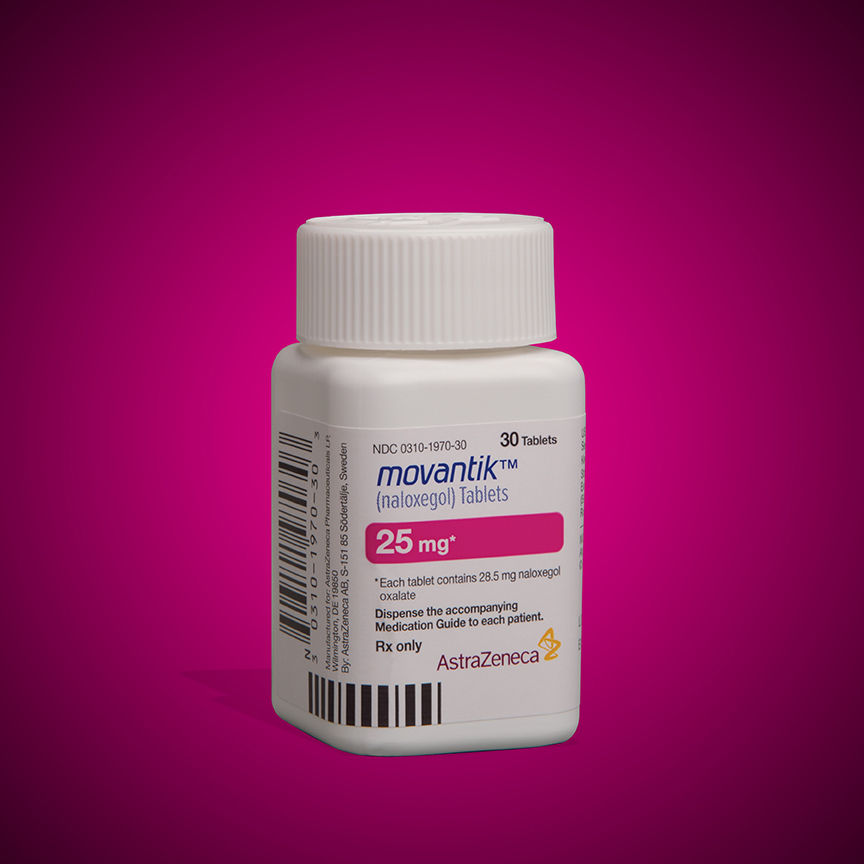
No results There are no results Quick relief of opioid-induced constipation with MNTXPam Harrison20 November 2020 Subcutaneous (MNTX) (Relister), an antagonist of peripheral μ-opioid receptors, relieves opioid induced (OID) in both chronic disease, not cancer-related, concludes a new analysis. "While these are two very different groups of patients, the ability to have something to treat OIC in non-cancer patients who remain in opioids for any reason helps, because [other] these patients are not doing well," said lead author Eric Shah, MD, Motility Director for Dartmouth, Dartmouth Hitchcock Health, Lebanon, New Hampshire. Importantly, μ-opioid receptor antagonists acting peripherally as MNTX do not affect overall pain control to any significant extent, which is "reasuring," Medscape Medical News said. These drugs reduce the constituencies of opioids without reversing the effects of the central nervous system—mediate opioids, he explained. "Methylnaltrexone has already been approved for the treatment of OIC in adults with noncancer chronic pain, as well as for OIC in adults with advanced disease who are receiving palliative care, which is often the case in patients with cancer-related pain," he said. Shah was discussing the new analysis during PAINWeek 2020, the American Society of Pain Medicine (ASRA) 19th Annual Meeting of Pain Medicine. The analysis was based on a review of the data collected in two randomized and placebo-controlled studies (Study 302 and 4000), which were used to obtain approval. The new analysis shows that "the drug works in front, and the effect is able to stay," he said. "I think studies are clinically relevant in that patients may have an intestinal movement quickly after giving them an injectable formulation when they are vomiting or otherwise cannot tolerate a pill and feel miserable," Shah said. Many OIC patients are constipated for reasons other than the use of opioids. They often have other side effects of opioids, including swelling, nausea and vomiting. "When patients go to the emergency room, it is not only that they cannot have an intestinal movement; often they also vomit, so it is important to have agents that can be given in a way that avoids the need for oral medications," Shah said. MNTX is the only opioid antagonist that acts peripherally available in a subcutaneous formulation. In addition, if patients can control these symptoms at home with injectable formulation, they may not need to go to the emergency department for the treatment of their gastrointestinal discomfort, he added. Visible product Approaching to comment, Darren Brenner, MD, associate professor of medicine and surgery, Northwestern University, Chicago, Illinois, who has worked with this subcutaneous formulation, said it is "definitely a viable product. "The data presented here were in patients with advanced disease who receive palliative care when others have failed, and the difference and potential benefit for MNTX is that it is the only peripheral receptor antagonist that acts μ-opioids that is approved for advanced cancer," he added. The other products that are currently approved (Movantik) and (Simproic), are indicated for chronic and non-cancer pain. The other potential benefit of subcutaneous MNTX is that it can work very quickly for patients who respond to it. "One of the things researchers did not mention in these two trials, but that has been shown in previous studies is that almost half of the patients who respond to this medication respond within the first 30 minutes of receiving the injection," Brenner told Medscape Medical News. This can be very beneficial in an emergency environment, as it can prevent patients from entering the hospital. They can be downloaded and sent home with enough drug to use on request, Brenner suggested. New study data analysis 302 and 4000 Both studies were conducted in adults with advanced disease and OIC whose conditions were refractory to laxative use. Both studies were controlled by placebo. The 302 study included 78 cancer patients and 56 patients with cancer-related COCIA. MNTX received a dose of 0.15 mg/kg subcutaneously every other day for 2 weeks. The 4000 study included 152 patients with cancer and OIC and 78 patients with OIC cancer-related non-cancer patients. In this study, the dose of MNTX was based on body weight. Seven or less doses of 8 mg or 12 mg were given subcutaneously for 2 weeks. The main endpoints of both studies were the proportion of patients who achieved a rescue-free response (RFL) within 4 hours after the first dose and the proportion of patients with RFL response within 4 hours for two or more of the first four doses within 24 hours. Shah explained that RFL is a significant clinical endpoint. Patients could achieve an intestinal movement with the two pre-spected final points in both studies. Not all patients were hospitalized for the OIC, Shah said. The entry criteria were strict and included having less than three bowel movements during the previous week and no clinically significant laxation (defecation) within 48 hours after receiving the first dose of study drug. "In both studies, a significantly higher proportion of patients treated with MNTX vs placebo achieved RFL within 4 hours after the first dose of cancer patients and noncancer," the researchers said. Table 1. Proportion of patients who achieved an RFL response within 4 hours of the first dose table 1. Proportion of patients who achieved an RFL response within 4 hours of the first dose Study 302 P value Study 4000 P value Cancer patients: MNTX 51.4 per cent 69.6% Patients with cancer: placebo 14.6% " Secc. 15.1 per cent " Seg.001 Noncancer patients: MNTX 44% 70.3% Noncancer patients: placebo 16.7% " Secc. 22% " Seg.001 Results were relatively comparable between cancer and non-cancer patients who were treated for OIC in the 4000 study, a note by researchers. Table 2. Repetition dosing with subcutaneous Mntx: RFL Response Within 4 hours for two or more of the first four injections, held at 24 hours Table 2. Repetition dosing with subcutaneous Mntx: RFL Response Within 4 hours for two or more of the first four injections, Staying at 24 hours Study 302 P value Study 4000 P value Cancer patients: MNTX 51.4 per cent 59.5% Patients with cancer: placebo 7.3% ≤0.0001 6.8% 0 Noncancer patients: MNTX 48% 70.3% Noncancer patients: placebo 10% ≤0.0001 14.6% 0 Both studies were sponsored by Salix Pharmaceuticals. Shah has received travel rates from Salix Pharmaceuticals. Brenner has been a consultant for Salix Pharmaceuticals, AstraZeneca and Purdue Pharma. AstraZeneca developed naloxegol. American Society of Regional Anesthesia and Pain Medicine (ASRA) 19th Annual Meeting of Pain Medicine: Summary 1347. Presented on 21 November 2020. Medscape Medical News © 2020 Send news tips to . Cite this: Fast relief of opioid-induced constipation with MNTX - Medscape - Nov 20, 2020.Autors and Disclosures Pam HarrisonComments Most popular items You have already selected for My AlertsClick the topic below to receive emails when new items are available. You've successfully added to your alerts. You will receive email when the new content is published. processing... COVID-19Help us make reference in Medscape the best clinical resource possible. about MembershipWebMD NetworkEditions
Opioid-Induced Constipation
Managing Opioid- Induced Constipation
Opioid-induced Constipation: Causes and Treatments
Opioid-Induced Constipation: Clinical Guidance and Approved Therapies
Pathophysiology, diagnosis, and management of opioid-induced constipation - The Lancet Gastroenterology & Hepatology
Opioid-Induced Constipation: Clinical Guidance and Approved Therapies
Opioid-induced Constipation: Causes and Treatments
Proposed algorithm for the treatment of opioid induced bowel... | Download Scientific Diagram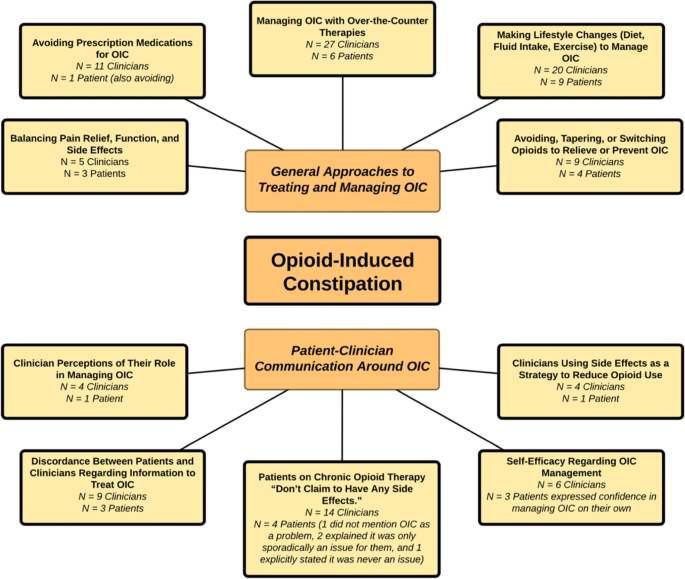
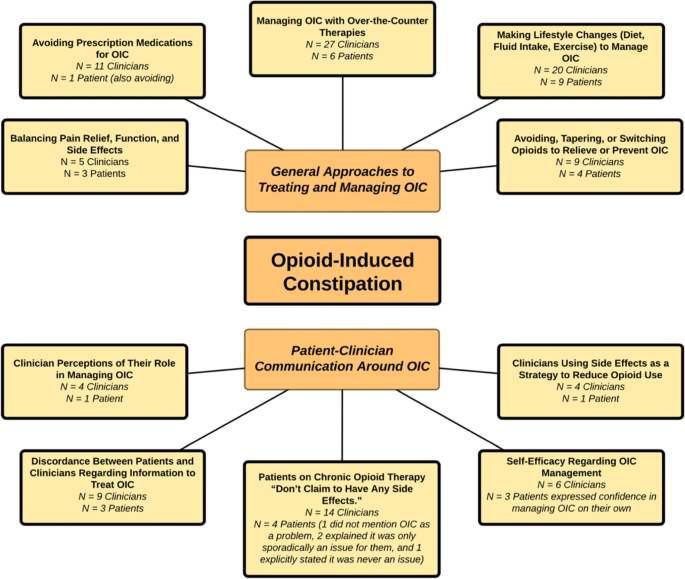
Patient and provider differences in the treatment of opioid-induced constipation: a qualitative study | BMC Gastroenterology | Full Text
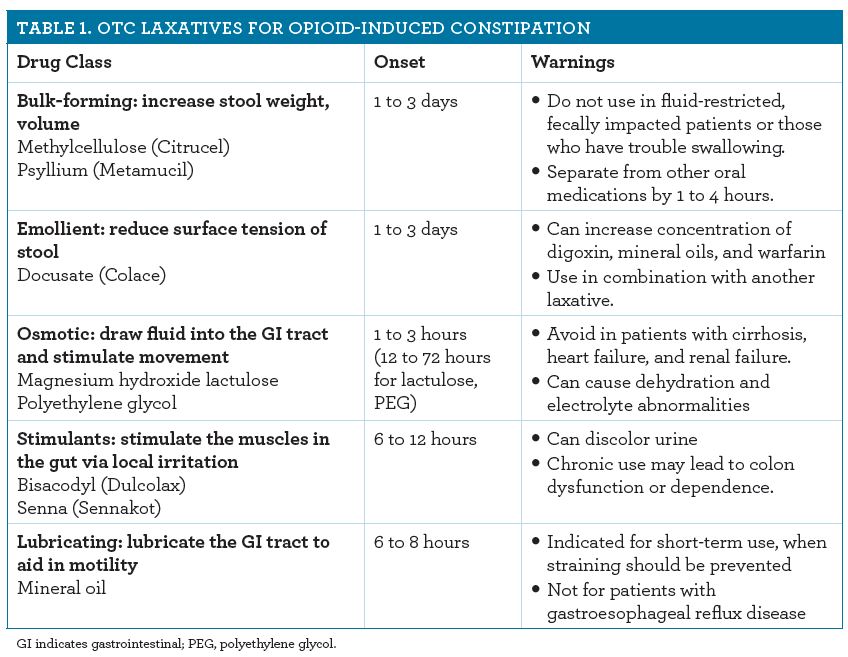
Management of Opioid-Induced Constipation
Opioid-Induced Constipation: New and Emerging Therapies—Update 2015
Methylnaltrexone and opioid-induced constipation
Pharmacological therapies for opioid induced constipation in adults with cancer | The BMJ
Opioid-induced Constipation: Causes and Treatments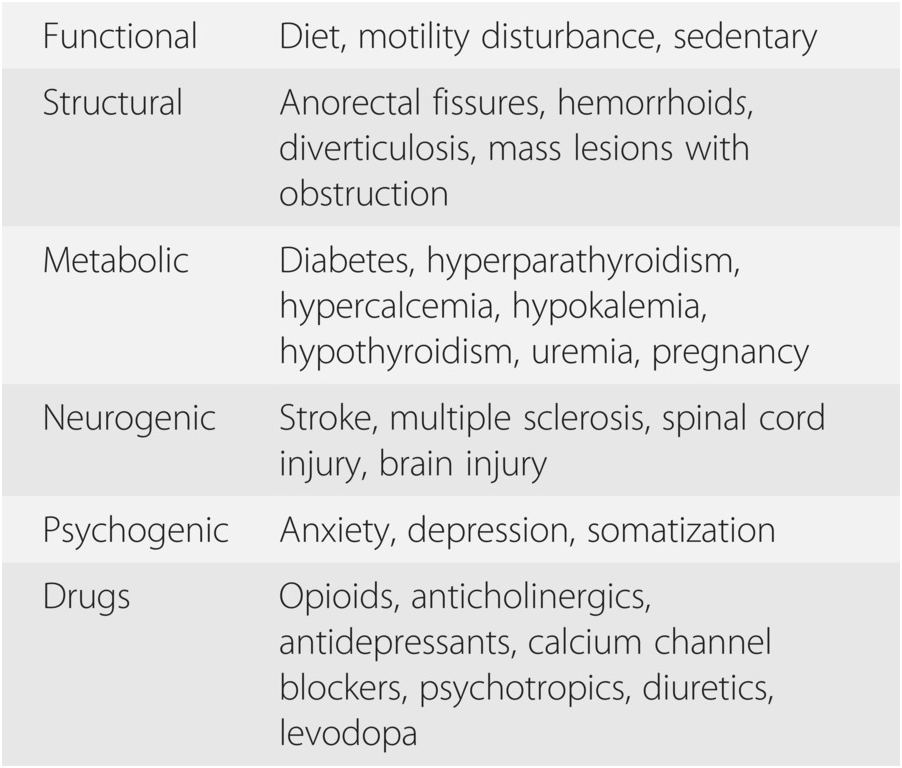
Opioid-induced constipation (Chapter 67) - Case Studies in Pain Management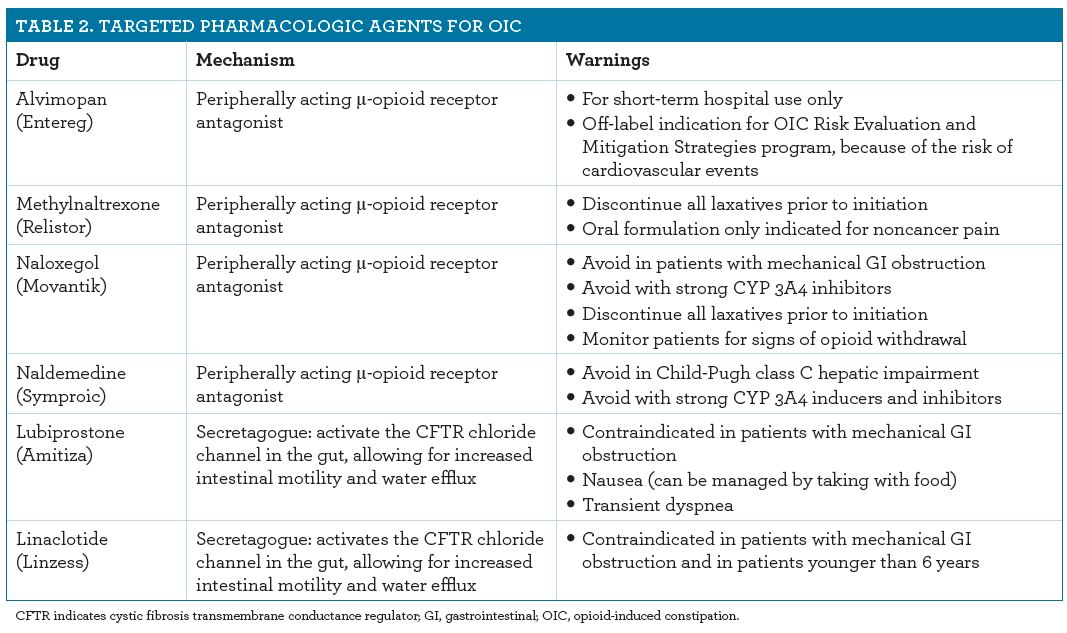
Opioid-Induced Constipation
Treatment of Opioid-Induced Constipation: The Hard Facts![PDF] New approaches to the treatment of opioid-induced constipation. | Semantic Scholar PDF] New approaches to the treatment of opioid-induced constipation. | Semantic Scholar](https://d3i71xaburhd42.cloudfront.net/f1c4a4ddd66511b824a7fdb374a6026758568e1b/4-Figure2-1.png)
PDF] New approaches to the treatment of opioid-induced constipation. | Semantic Scholar
Combating Opioid-Induced Constipation: New and Emerging Therapies
Management of Constipation in Older Adults - American Family Physician
Figure 3 from Opioid-induced constipation: advances and clinical guidance | Semantic Scholar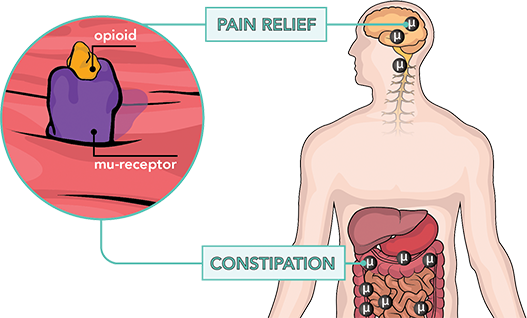
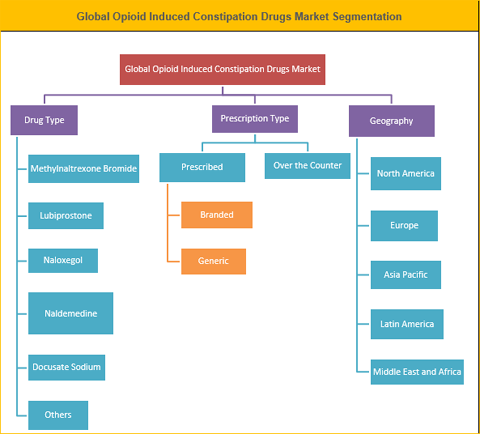
Opioid Induced Constipation Market Analysis, Top Companies, New Technology | by Pramod Kumar | Medium
China Opioid Induced Constipation Drugs Market Overview With Detailed Analysis, Competitive Landscape (2021-2027) – The Courier
Treating Opioid-Induced Constipation
Algorithm to treat opioid induced constipation and bowel dysfunction.... | Download Scientific Diagram
Slide Show - Understanding Opioid-Induced Constipation![Full text] Peripherally acting u-opioid receptor antagonists as treatment opti | PPA Full text] Peripherally acting u-opioid receptor antagonists as treatment opti | PPA](https://www.dovepress.com/cr_data/article_fulltext/s78000/78042/img/PPA-78042-F02.png)
Full text] Peripherally acting u-opioid receptor antagonists as treatment opti | PPA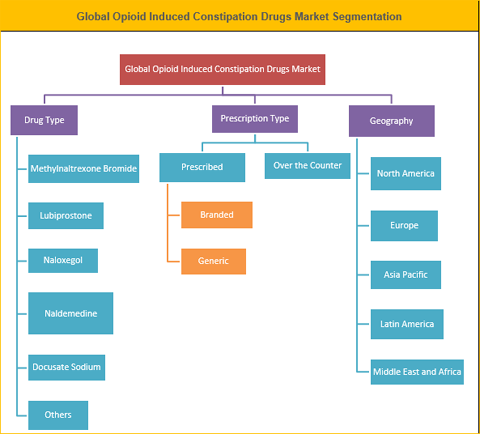
Opioid Induced Constipation (OIC) Drugs Market Size, Share And Forecast To 2026
Managing opioid-induced constipation
Opioid-Induced Constipation: New and Emerging Therapies—Update 2016
Asia Pacific Opioid Induced Constipation Drug Market | Forecast 2017-2025
Opioid-Induced Constipation: Pathophysiology, Clinical Consequences, and Management
Pathophysiology, diagnosis, and management of opioid-induced constipation - The Lancet Gastroenterology & Hepatology
Opioid-Induced Constipation: Insights Into Diagnosis and Effective Treatment - Clinical Pain Advisor
Opioid-induced constipation: Causes, symptoms, and treatment
Labeling Updated for Multiple Drugs Indicated for Opioid-Induced Constipation - MPR
MOVANTIK™ (naloxegol) Tablets for the Treatment of Opioid-Induced Constipation in Adult Patients with Chronic Non-Cancer Pain Launched in the US | Business Wire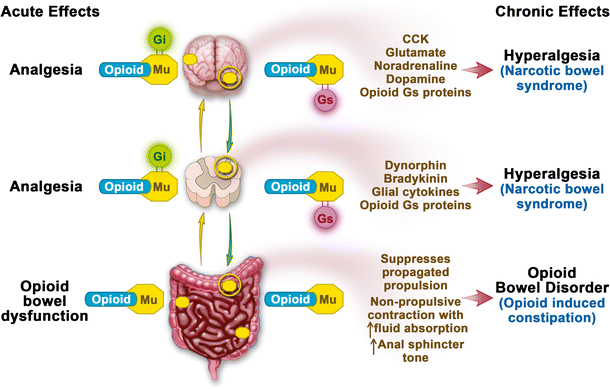
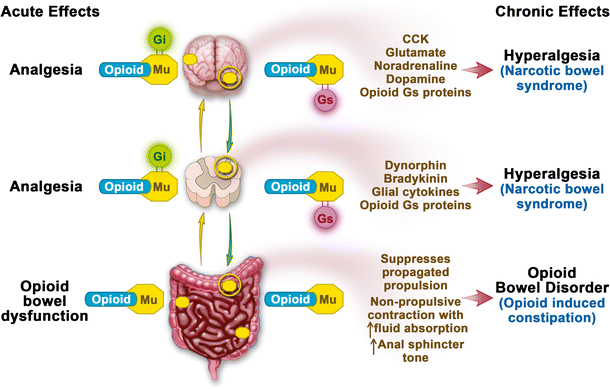
Narcotic Bowel Syndrome and Opioid-Induced Constipation | SpringerLink
Opioid-Induced Constipation Treatment: Medication and Remedies
 Opioid-Induced Constipation: New and Emerging Therapies—Update 2016
Opioid-Induced Constipation: New and Emerging Therapies—Update 2016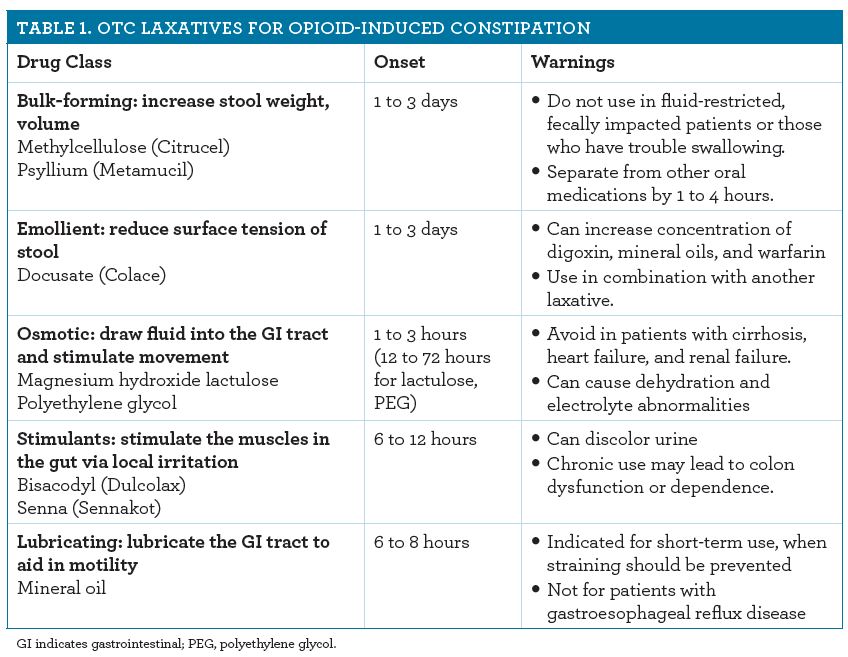











![PDF] New approaches to the treatment of opioid-induced constipation. | Semantic Scholar PDF] New approaches to the treatment of opioid-induced constipation. | Semantic Scholar](https://d3i71xaburhd42.cloudfront.net/f1c4a4ddd66511b824a7fdb374a6026758568e1b/4-Figure2-1.png)







![Full text] Peripherally acting u-opioid receptor antagonists as treatment opti | PPA Full text] Peripherally acting u-opioid receptor antagonists as treatment opti | PPA](https://www.dovepress.com/cr_data/article_fulltext/s78000/78042/img/PPA-78042-F02.png)








Posting Komentar untuk "opioid induced constipation drug"